Tuberc Respir Dis.
2012 Jan;72(1):24-29.
Annual Change of Peak Expiratory Flow Rate in Asthma and COPD
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. khyou@kuh.ac.kr
- 2Department of Internal Medicine, Konkuk University Chungju Hospital, Konkuk University School of Medicine, Chungju, Korea.
Abstract
- BACKGROUND
Measurement of peak expiratory flow rate (PEFR) in a follow-up examination for a chronic airway disease is useful because it has the advantages of being a simple measurement and can be repeated during examination. The aim of this study was to examine the annual decrease of PEFR in asthma and chronic obstructive pulmonary disease (COPD) patients and to confirm the factors which influence this decrease.
METHODS
From May, 2003 to September, 2010, the annual decrease of PEFR was obtained from asthma and COPD patients attending an outpatient pulmonary clinic. PEFR was measured using a Mini-Wright peak flow meter (Clement Clarke International Ltd. UK), and we conducted an analysis of factors that influence the change of PEFR and its average values.
RESULTS
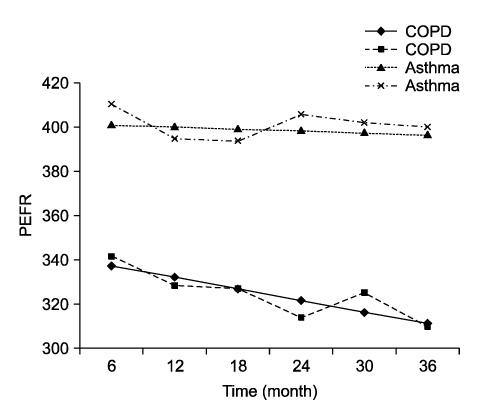
The results showed an annual decrease of 1.70+/-12.86 L/min the asthmatic patients and an annual decrease of 10.3+/-7.32 L/min in the COPD patients. Age and FEV1 were the predictive factors influencing change in asthma, and FEV1 and smoking were the predictive factors influencing change in COPD.
CONCLUSION
We confirmed the annual decreasing PEFR in patients with chronic airway disease and identified factors that work in conjunction with FEV1 to influence the change.
Keyword
MeSH Terms
Figure
Reference
-
1. Chang WC, Kim BK, Kim SJ, Yoo KH, Lee JY, Lee KY. The agreements between FEV1 and PEFR in the patients of mild bronchial asthma. Tuberc Respir Dis. 2005. 59:638–643.2. Fromer L, Cooper CB. A review of the GOLD guidelines for the diagnosis and treatment of patients with COPD. Int J Clin Pract. 2008. 62:1219–1236.3. Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977. 1:1645–1648.4. Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008. 359:1543–1554.5. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007. 176:532–555.6. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008. 31:143–178.7. American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995. 152:S77–S121.8. Croxton TL, Weinmann GG, Senior RM, Hoidal JR. Future research directions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002. 165:838–844.9. Ting S. Multicolored simplified asthma guideline reminder (MSAGR) for better adherence to national/global asthma guidelines. Ann Allergy Asthma Immunol. 2002. 88:326–330.10. Park MJ, Choi CW, Kim SJ, Kim YK, Lee SY, Kang KH, et al. Survey of COPD management among the primary care physicians in Korea. Tuberc Respir Dis. 2008. 64:109–124.11. Hegewald MJ, Crapo RO, Jensen RL. Intraindividual peak flow variability. Chest. 1995. 107:156–161.12. Gannon PF, Burge PS. Serial peak expiratory flow measurement in the diagnosis of occupational asthma. Eur Respir J Suppl. 1997. 24:57S–63S.13. Quanjer PH, Lebowitz MD, Gregg I, Miller MR, Pedersen OF. Peak expiratory flow: conclusions and recommendations of a Working Party of the European Respiratory Society. Eur Respir J Suppl. 1997. 24:2S–8S.14. Dahlqvist M, Eisen EA, Wegman DH, Kriebel D. Reproducibility of peak expiratory flow measurements. Occup Med. 1993. 8:295–302.15. Vaughan TR, Weber RW, Tipton WR, Nelson HS. Comparison of PEFR and FEV1 in patients with varying degrees of airway obstruction. Effect of modest altitude. Chest. 1989. 95:558–562.16. Meltzer AA, Smolensky MH, D'Alonzo GE, Harrist RB, Scott PH. An assessment of peak expiratory flow as a surrogate measurement of FEV1 in stable asthmatic children. Chest. 1989. 96:329–333.17. Gautrin D, D'Aquino LC, Gagnon G, Malo JL, Cartier A. Comparison between peak expiratory flow rates (PEFR) and FEV1 in the monitoring of asthmatic subjects at an outpatient clinic. Chest. 1994. 106:1419–1426.18. Contoli M, Baraldo S, Marku B, Casolari P, Marwick JA, Turato G, et al. Fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease: 5-year follow-up. J Allergy Clin Immunol. 2010. 125:830–837.19. Quanjer PH. A 10 year follow up of 180 adults with bronchial asthma: factors important for the decline in lung function. Thorax. 1992. 47:484.20. Kupczyk M, Kupryś I, Górski P, Kuna P. Long-term deterioration of lung function in asthmatic outpatients. Respiration. 2004. 71:233–240.21. Hesselink AE, van der Windt DA, Penninx BW, Wijnhoven HA, Twisk JW, Bouter LM, et al. What predicts change in pulmonary function and quality of life in asthma or COPD? J Asthma. 2006. 43:513–519.22. Kerstjens HA, Rijcken B, Schouten JP, Postma DS. Decline of FEV1 by age and smoking status: facts, figures, and fallacies. Thorax. 1997. 52:820–827.23. Jackson H, Hubbard R. Detecting chronic obstructive pulmonary disease using peak flow rate: cross sectional survey. BMJ. 2003. 327:653–654.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship of Chronic Obstructive Pulmonary Disease (COPD) to Asthma
- A study of predicted values of peak expiratory flow rates in primary school children
- An Evaluation of the Accuracy of Mini-Wright Peak Flowmeters in Patients with Asthma and Chronic Obstructive Pulmonary Disease
- Comparison of Mini-Wright Peak Flow Meter and Microplus Pocket Spirometer in Measuring Peak Expiratory Flow Rate
- A Study on Predicted Values of Peak Expiratory Flow Rate in Primary School Children