Tuberc Respir Dis.
2010 Dec;69(6):418-425.
Long-Term Effects of ACE Inhibitors in Post-Tuberculosis Emphysema
- Affiliations
-
- 1Department of Internal Medicine, Seoul Metropolitan Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. heechung@snu.ac.kr
Abstract
- BACKGROUND
Little is known about the long-term effects of angiotensin-converting enzyme (ACE) treatment on post-tuberculosis emphysema. This study evaluated the effects of ACE inhibition on cardiac function and gas exchange in patients with post-tuberculosis emphysema.
METHODS
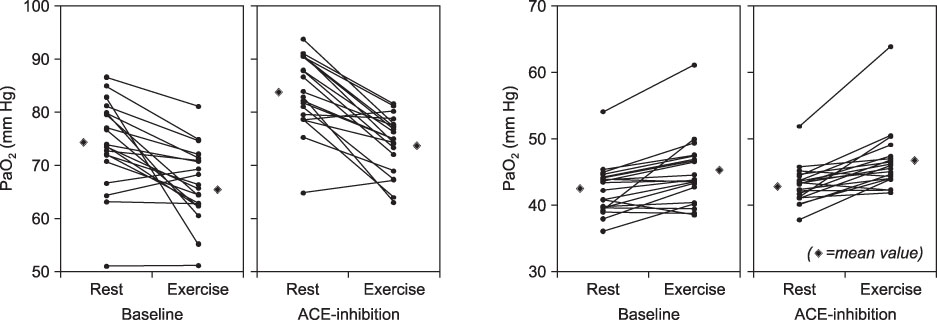
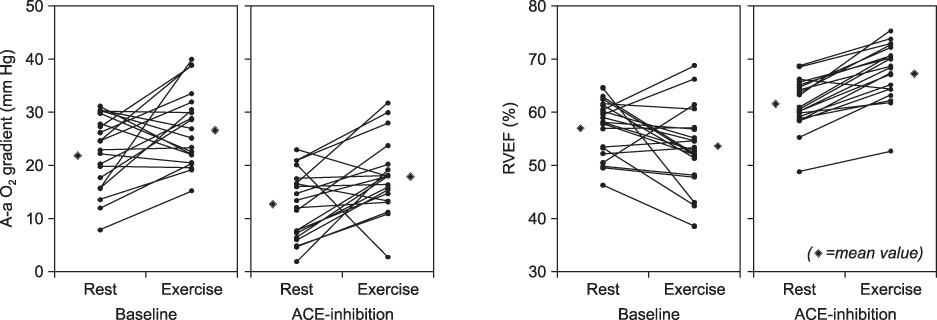
At baseline and at 6 months after initiation of ACE inhibition therapy, patients underwent pulmonary function testing, arterial blood gas analysis, and echocardiography, both at rest and post exercise. Cardiac output (CO) and right ventricular ejection fraction (RVEF) were measured at those time points as well.
RESULTS
After ACE inhibition; resting and post-exercise RVEF (Mean+/-SEM, 61.5+/-1.0, 67.6+/-1.2%, respectively) were higher than at baseline (56.9+/-1.2, 53.5+/-1.7%). Resting and post-exercise CO (6.37+/-0.24, 8.27+/-0.34 L/min) were higher than at baseline (5.42+/-0.22, 6.72+/-0.24 L/min). Resting and post-exercise PaO2 (83.8+/-1.6, 74.0+/-1.2 mmHg, respectively) were also higher than at baseline (74.2+/-1.9, 66.6+/-1.6 mmHg). Post-exercise PaCO2 (46.3+/-1.1 mmHg) was higher than at baseline (44.9+/-1.1; Resting 42.8+/-0.8 vs. 42.4+/-0.9 mmHg). Resting and post-exercise A-a O2 gradient (12.4+/-1.4, 17.8+/-1.5 mmHg) were lower than at baseline (22.5+/-1.5, 26.9+/-1.6 mmHg).
CONCLUSION
In post-tuberculosis emphysema, RVEF and CO were augmented with a resultant increase in peripheral oxygen delivery after ACE inhibition. These findings suggest that an ACE inhibitor may have the potential to alleviate co-morbid cardiac conditions and benefit the patients with post-tuberculosis emphysema.
MeSH Terms
Figure
Reference
-
1. Kim MA, Kim SH, Zo JH, Hwangbo B, Lee JH, Chung HS. Right heart dysfunction in post-tuberculosis emphysema. Int J Tuberc Lung Dis. 2004. 8:1120–1126.2. Nong Z, Stassen JM, Moons L, Collen D, Janssens S. Inhibition of tissue angiotensin-converting enzyme with quinapril reduces hypoxic pulmonary hypertension and pulmonary vascular remodeling. Circulation. 1996. 94:1941–1947.3. Mancini GB, Etminan M, Zhang B, Levesque LE, FitzGerald JM, Brophy JM. Reduction of morbidity and mortality by statins, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers in patients with chronic obstructive pulmonary disease. J Am Coll Cardiol. 2006. 47:2554–2560.4. Cazzola M, Matera MG, Rogliani P, Page C. Treating systemic effects of COPD. Trends Pharmacol Sci. 2007. 28:544–550.5. Mortensen EM, Copeland LA, Pugh MJ, Restrepo MI, de Molina RM, Nakashima B, et al. Impact of statins and ACE inhibitors on mortality after COPD exacerbations. Respir Res. 2009. 10:45.6. Schlueter DP, Immekus J, Stead WW. Relationship between maximal inspiratory pressure and total lung capacity (coefficient of retraction) in normal subjects and in patients with emphysema, asthma, and diffuse pulmonary infiltration. Am Rev Respir Dis. 1967. 96:656–665.7. American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991. 144:1202–1218.8. Poppius H. Airway obstruction in pulmonary tuberculosis. Scand J Respir Dis Suppl. 1968. 65:165–169.9. Birath G, Caro J, Malmberg R, Simonsson BG. Airways obstruction in pulmonary tuberculosis. Scand J Respir Dis. 1966. 47:27–36.10. Snider GL, Doctor L, Demas TA, Shaw AR. Obstructive airway disease in patients with treated pulmonary tuberculosis. Am Rev Respir Dis. 1971. 103:625–640.11. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2009. Washington: Medical Communications Resources.12. Rubin LJ. Cardiovascular effects of vasodilator therapy for pulmonary arterial hypertension. Clin Chest Med. 1983. 4:309–319.13. Matthay RA, Arroliga AC, Wiedemann HP, Schulman DS, Mahler DA. Right ventricular function at rest and during exercise in chronic obstructive pulmonary disease. Chest. 1992. 101:255S–262S.14. Vizza CD, Lynch JP, Ochoa LL, Richardson G, Trulock EP. Right and left ventricular dysfunction in patients with severe pulmonary disease. Chest. 1998. 113:576–583.15. Schulman DS, Matthay RA. The right ventricle in pulmonary disease. Cardiol Clin. 1992. 10:111–135.16. Matthay RA, Niederman MS, Wiedemann HP. Cardiovascular-pulmonary interaction in chronic obstructive pulmonary disease with special reference to the pathogenesis and management of cor pulmonale. Med Clin North Am. 1990. 74:571–618.17. Willenheimer R, Rydberg E, Oberg L, Juul-Möller S, Erhardt L. ACE inhibition with ramipril improves left ventricular function at rest and post exercise in patients with stable ischaemic heart disease and preserved left ventricular systolic function. Eur Heart J. 1999. 20:1647–1656.18. van Suylen RJ, Smits JF, Daemen MJ. Pulmonary artery remodeling differs in hypoxia- and monocrotaline-induced pulmonary hypertension. Am J Respir Crit Care Med. 1998. 157:1423–1428.19. Dandona P, Dhindsa S, Ghanim H, Chaudhuri A. Angiotensin II and inflammation: the effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockade. J Hum Hypertens. 2007. 21:20–27.20. Busquets X, MacFarlane NG, Heine-Suñer D, Morlá M, Torres-Juan L, Iglesias A, et al. Angiotensin-converting-enzyme gene polymorphisms, smoking and chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2007. 2:329–334.21. Barnes PJ. Future treatments for chronic obstructive pulmonary disease and its comorbidities. Proc Am Thorac Soc. 2008. 5:857–864.22. Klinger JR, Hill NS. Right ventricular dysfunction in chronic obstructive pulmonary disease. Evaluation and management. Chest. 1991. 99:715–723.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Difference in Right Ventricular Function between Post-tuberculosis Emphysema and Primary Emphysema
- Angiotensin Converting Enzyme (ACE) in Serum and Bronchoalveolar Lavage (BAL) Fluid in Patients with Active Pulmonary Tuberculosis
- A Study on Angiotensin Converting Enzyne Activity in Pulmonary Tuberculosis
- A case of endobronchial tuberculosis accompanied with obstructive emphysema
- The Effect of Proton Pump Inhibitors on Nutrition, Metabolism, Infection and Small Intestinal Bacterial Overgrowth: Safe Perspective