Tuberc Respir Dis.
2010 Apr;68(4):231-235.
A Case of Node-bronchial Fistula by Non-small Cell Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea. cem@ewha.ac.kr
- 2Department of Radiology, Ewha Womans University School of Medicine, Seoul, Korea.
Abstract
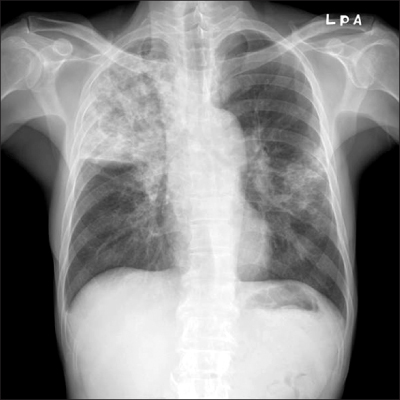
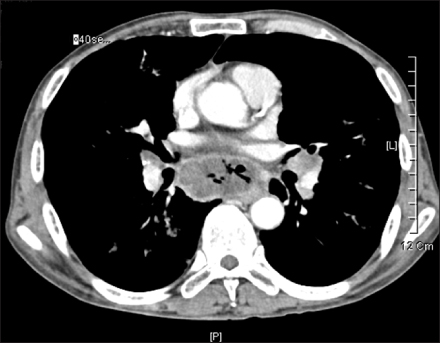
- Lymphadenopathy in the thoracic cavity is frequently caused by inflammatory diseases. In very rare cases, the node-bronchial fistula has been reported to be the cause of complications of pulmonary tuberculosis. A male patient with necrotizing pneumonia and mediastinal lymph node enlargements identified by chest computed tomography was also found to have a node-bronchial fistula caused by lung cancer. The patient was treated for tuberculosis with pneumonia for one week before a definitive diagnosis was made. A further investigation revealed him to have non-small cell lung cancer (NSCLC, adenocarcinoma) and multiple mediastinal lymphadenopathies accompanied with the node-bronchial fistula. We report this specific case that had been previously treated for tuberculosis but was later revealed to be NSCLC accompanied with a node-bronchial fistula.
Keyword
MeSH Terms
Figure
Reference
-
1. Im JG, Lee KS. The chest radiology. 2000. 1st ed. Seoul: Ilchokak.2. Iselin H, Suter F. The role of perforation of hilar lymph nodes into the bronchial tree of adults. Chest. 1954. 25:302–311.3. Jiang B, Wu GP, Zhao YJ, Wang SC. Transcription expression and clinical significance of TTF-1 mRNA in pleural effusion of patients with lung cancer. Diagn Cytopathol. 2008. 36:849–854.4. Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest. 1997. 111:1718–1723.5. Lois M, Noppen M. Bronchopleural fistulas: an overview of the problem with special focus on endoscopic management. Chest. 2005. 128:3955–3965.6. Park EH, Jang TW, Park MI, Song JY, Choi IS, Oak CH, et al. A case of esophago-mediatinal fistula due to esophageal tuberculosis. Tuberc Respir Dis. 2007. 62:531–535.7. Gu P, Zhao YZ, Jiang LY, Zhang W, Xin Y, Han BH. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer. 2009. 45:1389–1396.8. Zwischenberger JB, Savage C, Alpard SK, Anderson CM, Marroquin S, Goodacre BW. Mediastinal transthoracic needle and core lymph node biopsy: should it replace mediastinoscopy? Chest. 2002. 121:1165–1170.9. Wang MZ, Wan XB, Chen Y, Zhang L, Zhong W, Zhong X, et al. The results of transbronchial needle aspiration in 164 cases with enlarged mediastinal and/or hilar lymph nodes. Zhonghua Nei Ke Za Zhi. 2009. 48:133–135.10. Fritscher-Ravens A, Bohuslavizki KH, Brandt L, Bobrowski C, Lund C, Knofel WT, et al. Mediastinal lymph node involvement in potentially resectable lung cancer: comparison of CT, positron emission tomography, and endoscopic ultrasonography with and without fine-needle aspiration. Chest. 2003. 123:442–451.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal Broncho-Mediastinal Fistula in a Patient with Non-Small Cell Lung Cancer after Photodynamic Therapy
- Coronary Fistula Anastomosing between Right Coronary Artery and Left Bronchial Artery Accompanied with Cystic Lung Disease
- Morphometric Analysis for Pulmonary Small Cell Carcinoma Using Image Analysis
- Coronary-to-Bronchial Artery Fistula Originating from the S-Shaped Sinoatrial Node Artery: CT and Angiography Findings
- Expression of p53 and nm23 Proteins in Non-Small Cell Lung Cancer