Tuberc Respir Dis.
2009 Dec;67(6):491-498.
Treatment Guidelines of Sepsis and Septic Shock
- Affiliations
-
- 1Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea. lhbmd@jbnu.ac.kr
Abstract
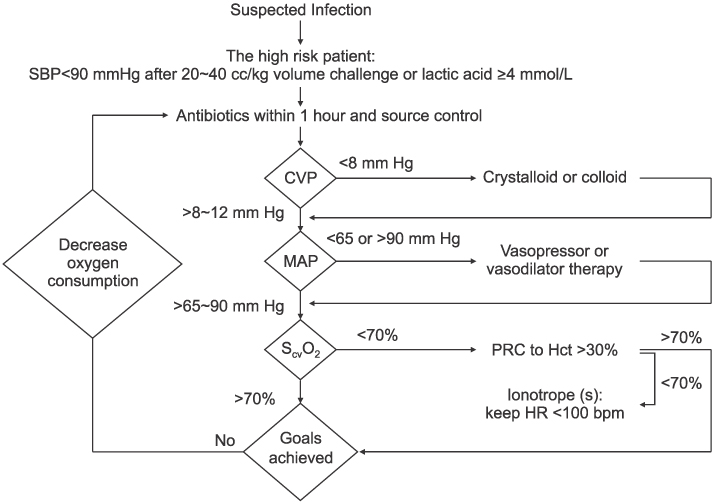
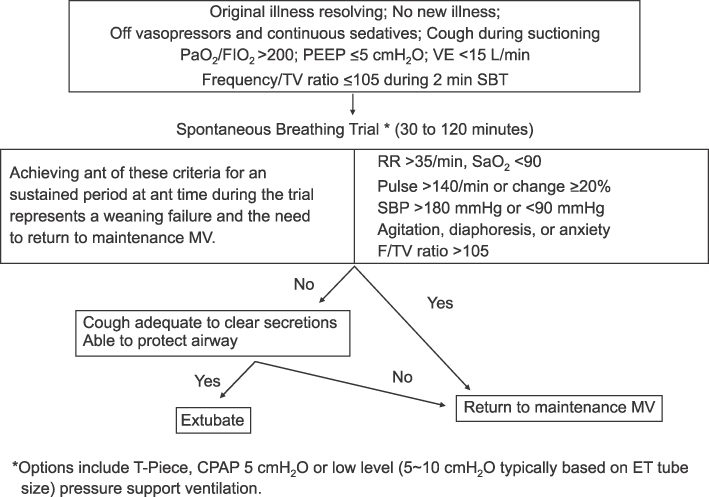
- Severe sepsis and septic shock are major healthcare problems with high mortality, ranging from 20% to 60%, affecting millions of individuals around the world each year. The speed and appropriateness of therapy administered in the initial hours after severe sepsis develops have an important impact on the outcome. In 2004, an international guideline that the bedside clinician could use to improve the outcomes in severe cases of sepsis and septic shock was published. Several landmark studies recently demonstrated that therapeutic strategies may reduce mortality substantially. The "Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock: 2008", using a new evidence-based methodology system for assessing the quality of evidence and the strength of the recommendations, was updated. The revised version is based on an updated search into 2007. Evidenced-based recommendations regarding the acute management of sepsis and septic shock are the first step toward improving the outcomes of critically ill patients. We review the treatment guidelines of sepsis and septic shock.
Keyword
MeSH Terms
Figure
Reference
-
1. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003. 348:1546–1554.2. Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007. 35:1244–1250.3. Matot I, Sprung CL. Definition of sepsis. Intensive Care Med. 2001. 27:Suppl 1. S3–S9.4. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign Management Guidelines Committee. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004. 32:858–873.5. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004. 328:1490.6. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008. 36:296–327.7. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992. 101:1644–1655.8. Carswell EA, Old LJ, Kassel RL, Green S, Fiore N, Williamson B. An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci U S A. 1975. 72:3666–3670.9. Tracey KJ, Beutler B, Lowry SF, Merryweather J, Wolpe S, Milsark IW, et al. Shock and tissue injury induced by recombinant human cachectin. Science. 1986. 234:470–474.10. Calandra T, Froidevaux C, Martin C, Roger T. Macrophage migration inhibitory factor and host innate immune defenses against bacterial sepsis. J Infect Dis. 2003. 187:Suppl 2. S385–S390.11. Fritz JH, Girardin SE, Fitting C, Werts C, Mengin-Lecreulx D, Caroff M, et al. Synergistic stimulation of human monocytes and dendritic cells by Toll-like receptor 4 and NOD1- and NOD2-activating agonists. Eur J Immunol. 2005. 35:2459–2470.12. Zingarelli B. Nuclear Factor-kappa B. Crit Care Med. 2005. 33:Suppl 12. S414–S416.13. Levi M, ten Cate H, van der Poll T, van Deventer SJ. Pathogenesis of disseminated intravascular coagulation in sepsis. JAMA. 1993. 270:975–979.14. Coopersmith CM, Chang KC, Swanson PE, Tinsley KW, Stromberg PE, Buchman TG, et al. Overexpression of Bcl-2 in the intestinal epithelium improves survival in septic mice. Crit Care Med. 2002. 30:195–201.15. Spronk PE, Zandstra DF, Ince C. Bench-to-bedside review: sepsis is a disease of the microcirculation. Crit Care. 2004. 8:462–468.16. Landry DW, Levin HR, Gallant EM, Ashton RC Jr, Seo S, D'Alessandro D, et al. Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation. 1997. 95:1122–1125.17. Schein RM, Sprung CL, Marcial E, Napolitano L, Chernow B. Plasma cortisol levels in patients with septic shock. Crit Care Med. 1990. 18:259–263.18. Slag MF, Morley JE, Elson MK, Crowson TW, Nuttall FQ, Shafer RB. Hypothyroxinemia in critically ill patients as a predictor of high mortality. JAMA. 1981. 245:43–45.19. Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest. 2006. 130:1579–1595.20. Esteban A, Alía I, Tobin MJ, Gil A, Gordo F, Vallverdú I, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. 1999. 159:512–518.21. Esteban A, Alía I, Gordo F, Fernández R, Solsona JF, Vallverdú I, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. 1997. 156:459–465.22. Brochard L, Rauss A, Benito S, Conti G, Mancebo J, Rekik N, et al. Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation. Am J Respir Crit Care Med. 1994. 150:896–903.23. Connors AF Jr, McCaffree DR, Gray BA. Evaluation of right-heart catheterization in the critically ill patient without acute myocardial infarction. N Engl J Med. 1983. 308:263–267.24. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001. 345:1368–1377.