Tuberc Respir Dis.
2009 Oct;67(4):364-368.
A Case of Bronchiolitis Interstitial Pneumonitis
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. yskwon@chonnam.ac.kr
- 2Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Chonnam National University Medical School, Gwangju, Korea.
- 4Department of Radiology, Chonnam National University Medical School, Gwangju, Korea.
Abstract
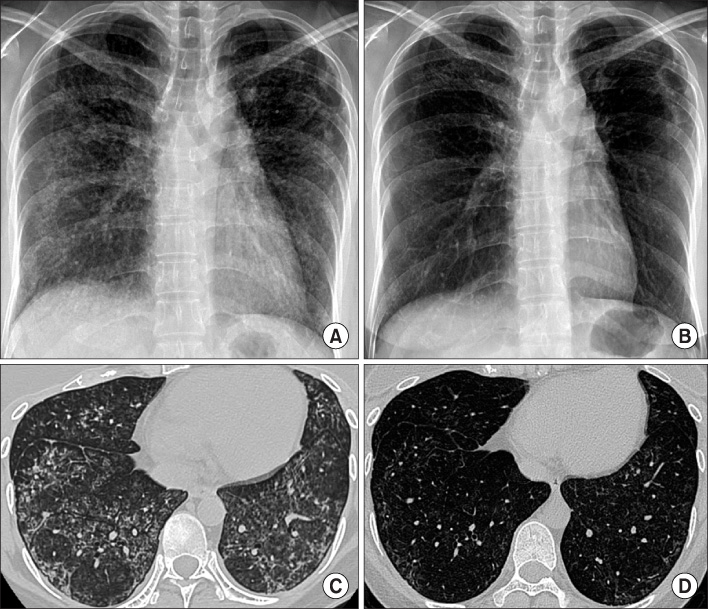
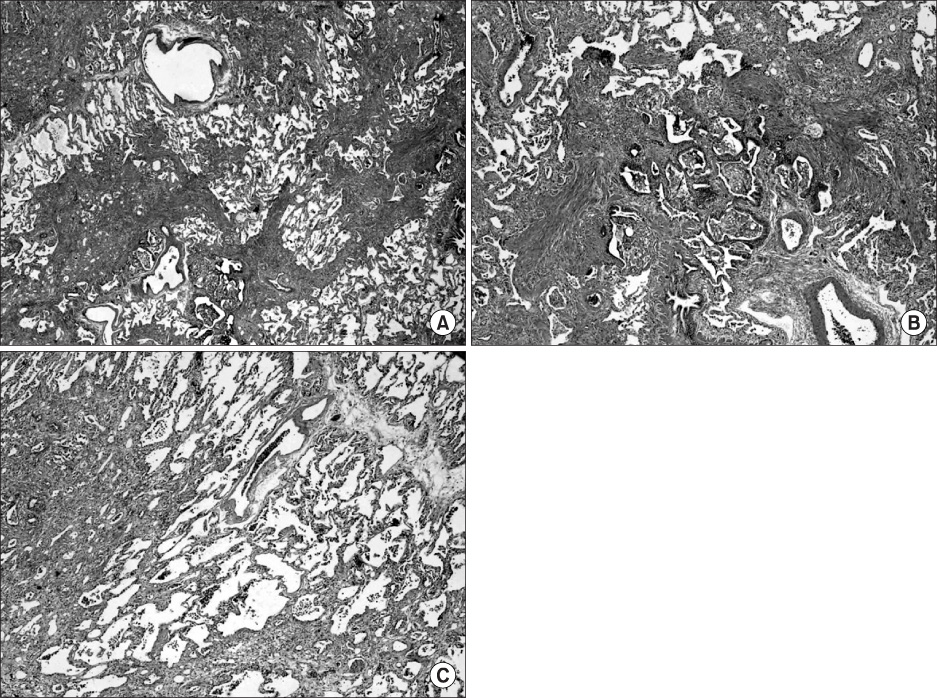
- Bronchiolitis interstitial pneumonitis (BIP), an unclassified and newly described interstitial pneumonia, has a combined feature of prominent bronchiolitis, interstitial inflammation, and fibrosis. It is distinct from bronchiolitis obliterans or bronchiolitis obliterans organizing pneumonia (BOOP). BIP has a better prognosis than common cases of interstitial pneumonia. However, BIP has a poorer prognosis than BOOP. BIP's response to corticosteroids is not as successful as BOOP's response to this treatment. We encountered the case of a 31-year-old woman with BIP with an initial presentation of dyspnea and a cough that had lasted for 3 months. The patient's chest CT scan demonstrated patchy ground glass opacities and multiple ill-defined centrilobular nodules in both lungs, suggesting military tuberculosis or nontuberculous mycobacterial infection. A video-assisted thoracoscopic lung biopsy resulted in the diagnosis of BIP. Clinical symptoms, pulmonary lesions, and pulmonary function tests were improved after oral glucocorticoid therapy.
MeSH Terms
Figure
Reference
-
1. David M Mitchell, Ashley Woodcock. The diagnosis, assessment and treatment of diffuse parenchymal lung disease in adults. Introduction. Thorax. 1999. 54:Suppl 1. S1–S14.2. American Thoracic Society. European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002. 165:277–304.3. Churg A, Myers J, Suarez T, Gaxiola M, Estrada A, Mejia M, et al. Airway-centered interstitial fibrosis: a distinct form of aggressive diffuse lung disease. Am J Surg Pathol. 2004. 28:62–68.4. Fukuoka J, Franks TJ, Colby TV, Flaherty KR, Galvin JR, Hayden D, et al. Peribronchiolar metaplasia: a common histologic lesion in diffuse lung disease and a rare cause of interstitial lung disease: clinicopathologic features of 15 cases. Am J Surg Pathol. 2005. 29:948–954.5. Mark EJ, Ruangchira-urai R. Bronchiolitis interstitial pneumonitis: a pathologic study of 31 lung biopsies with features intermediate between bronchiolitis obliterans organizing pneumonia and usual interstitial pneumonitis, with clinical correlation. Ann Diagn Pathol. 2008. 12:171–180.6. Yousem SA, Dacic S. Idiopathic bronchiolocentric interstitial pneumonia. Mod Pathol. 2002. 15:1148–1153.7. Qureshi RA, Ahmed TA, Grayson AD, Soorae AS, Drakeley MJ, Page RD. Does lung biopsy help patients with interstitial lung disease? Eur J Cardiothorac Surg. 2002. 21:621–626. discussion 626.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bronchiolitis Interstitial Pneumonitis
- A Case of Methotrexate Induced Pneumonitis in a Patient with Rheumatoid Arthritis
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Clinical Spectrum and Lung Pathology in Children with Interstitial Lung Disease
- A case of bronchiolitis obliterans organizing pneumonia in patient with systemic lupus erythematosus