Tuberc Respir Dis.
2008 Sep;65(3):198-206.
Comparison of a Closed with an Open Endotracheal Suction: Costs and the Incidence of Ventilator-associated Pneumonia
- Affiliations
-
- 1Department of Internal Medicine, ChungAng University College of Medicine, Seoul, Korea. jykimmd@cau.ac.kr
- 2Department of Medical Intensive Care Unit, ChungAng University Hospital, Seoul, Korea.
Abstract
-
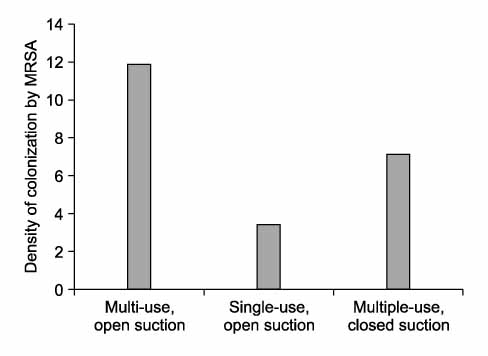
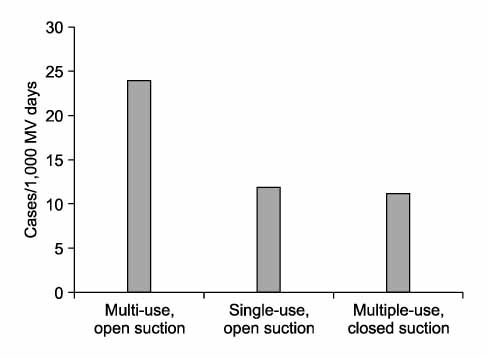
BACKGROUND: Tracheobronchial suctioning using the closed suctioning system has physiological benefits for critically ill patients. Despite these benefits, there are concerns about increased colonization of tracheobronchial tree by pathogenic organisms. The cost is another hinder to the introduction of closed suction system. The aim of this study was to evaluate the incidence of colonization and ventilator associated pneumonia and the cost-effectiveness of closed suction compared with open suction.
METHODS
During separated one month period, patients admitted MICU were cared by multiple-use, open suction, single-use, open suction and multiple-use, closed suction method, consecutively. Costs, colonization of tracheobronchial tree by MRSA and the incidence of ventilator-associated pneumonia (VAP) were analyzed.
RESULTS
One-hundred and six patients were enrolled. Twenty patients were treated with multiple-use, open suction, while 42 and 44 patients were cared with single-use, open catheter and multiple-use, closed catheter, respectively. Colonization by MRSA and the incidence of VAP were not different among three ways of suctioning. The overall costs per patient per day for suctioning were 10.58 dollars for multiple-use, open suction, 28.27 dollars for single-use, open suction and 23.76 dollars for multiple-use, closed suction.
CONCLUSION
Multiple-use, closed suctioning, when suction catheters were changed every 48 hrs, has the similar incidence of colonization of MRSA and occurrence of VAP and is a cost-efficient way of endotracheal suction.
MeSH Terms
Figure
Reference
-
1. Craig CK, Benson MS, Pierson DJ. Prevention of arterial oxygen desaturation during closed airway endotracheal suctioning: effect of ventilator mode. Respir Care. 1984. 29:1013–1018.2. Skelley BF, Deeren SM, Powaser MM. The effectiveness of two preoxygenation methods to prevent endotracheal suction-induced hypoxemia. Heart Lung. 1980. 9:316–323.3. Walsh JM, Vanderwarf C, Hoscheit D, Fahey PJ. Unsuspected hemodynamic alterations during endotracheal suctioning. Chest. 1989. 95:162–165.4. Clark AP, Winslow EH, Tyler DO, White KM. Effects of endotracheal suctioning on mixed venous oxygen saturation and heart rate in critically ill adults. Heart Lung. 1990. 19:552–557.5. Shim C, Fine N, Fernandez R, Williams MH Jr. Cardiac arrhythmias resulting from tracheal suctioning. Ann Intern Med. 1969. 71:1149–1153.6. Durand M, Sangha B, Cabal LA, Hoppenbrouwers T, Hodgman JE. Cardiopulmonary and intracranial pressure changes related to endotracheal suctioning in preterm infants. Crit Care Med. 1989. 17:506–510.7. Choong K, Chatrkaw P, Frndova H, Cox PN. Comparison of loss in lung volume with open versus in-line catheter endotracheal suctioning. Pediatr Crit Care Med. 2003. 4:69–73.8. Cobley M, Atkins M, Jones PL. Environmental contamination during tracheal suction: a comparison of disposable conventional catheters with a multiple-use closed system device. Anaesthesia. 1991. 46:957–961.9. Bodai BI. A means of suctioning without cardiopulmonary depression. Heart Lung. 1982. 11:172–176.10. Cordero L, Sananes M, Ayers LW. Comparison of a closed (Trach Care MAC) with an open endotracheal suction system in small premature infants. J Perinatol. 2000. 20:151–156.11. Combes P, Fauvage B, Oleyer C. Nosocomial pneumonia in mechanically ventilated patients, a prospective randomized evaluation of the Stericath closed suctioning system. Intensive Care Med. 2000. 26:878–882.12. Deppe SA, Kelly JW, Thoi LL, Chudy JH, Longfield RN, Ducey JP, et al. Incidence of colonization, nosocomial pneumonia, and mortality in critically ill patients using a Trach Care closed-suction system versus an open-suction system: prospective, randomized study. Crit Care Med. 1990. 18:1389–1393.13. Canadian Critical Care Trials Group. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N Engl J Med. 2006. 355:2619–2630.14. Kollef MH. The prevention of ventilator-associated pneumonia. N Engl J Med. 1999. 340:627–634.15. Kerem E, Yatsiv I, Goitein KJ. Effect of endotracheal suctioning on arterial blood gases in children. Intensive Care Med. 1990. 16:95–99.16. DePew C, Moseley M, Clark EG, Morales CC. Open versus closed-system endotracheal suctioning: as cost comparison. Crit Care Nurse. 1994. 14:94–100.17. Lorente L, Lecuona M, Jimenez A, Mora ML, Sierra A. Tracheal suction by closed system without daily change versus open system. Intensive Care Med. 2006. 32:538–544.18. Sole ML, Poalillo FE, Byers JF, Ludy JE. Bacterial growth in secretions and on suctioning equipment of orally in tubated patients: a pilot study. Am J Crit Care. 2002. 11:141–149.19. Ritz R, Scott LR, Coyle MB, Pierson DJ. Contamination of a multiple-use suction catheter in a closed-circuit system compared to contamination of a disposable, single-use suction catheter. Respir Care. 1986. 31:1086–1091.20. Rello J, Quintana E, Ausina V, Castella J, Luquin M, Net A, et al. Incidence, etiology and outcome of nosocomial pneumonia in mechanically ventilated patients. Chest. 1991. 100:439–444.21. Fagon JY, Chastre J, Domart Y, Trouillet JL, Pierre J, Darne C, et al. Nosocomial pneumonia in patients receiving continuous mechanical ventilation: prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Am Rev Respir Dis. 1989. 139:877–884.22. Johnson KL, Kearney PA, Johnson SB, Niblett JB, MacMillan NL, McClain RE. Closed versus open endotracheal suctioning: costs and physiologic consequences. Crit Care Med. 1994. 22:658–666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of Colonization, Ventilator-Associated Pneumonia as Related to the Type of Endotracheal Suction System in Mechanically Ventilated Patients
- Endotracheal Colonization and Ventilator-associated Pneumonia in Mechanically Ventilated Patients according to Type of Endotracheal Suction System
- Comparison of the Pattern in Semi-Quantitative Sputum Cultures Based on Different Endotracheal Suction Techniques
- A Comparison of the Opened Versus Closed-System of Suctioning : In Oxygen Saturation, Vital Signs and Suction Time
- Effects of a Closed Endotracheal Suction System on Oxygen Saturation, Ventilator-Associated Pneumonia, and Nursing Efficacy