Tuberc Respir Dis.
2008 Jun;64(6):451-455.
A Case of Angio-invasive Pulmonary Mucormycosis with Uncontrolled Diabetes Mellitus
- Affiliations
-
- 1Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Gyeongsang National University College of Medicine, Jinju, Korea. ljd8611@empal.com
- 2Department of Thoracic and Cardiovascular Surgery, Gyeongsang National University College of Medicine, Jinju, Korea.
Abstract
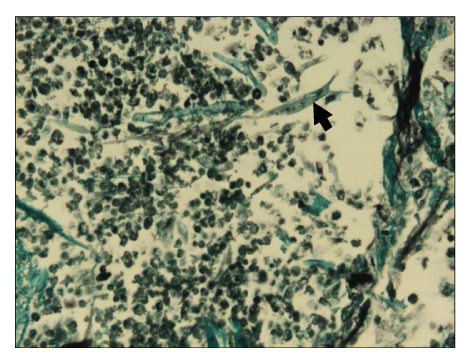
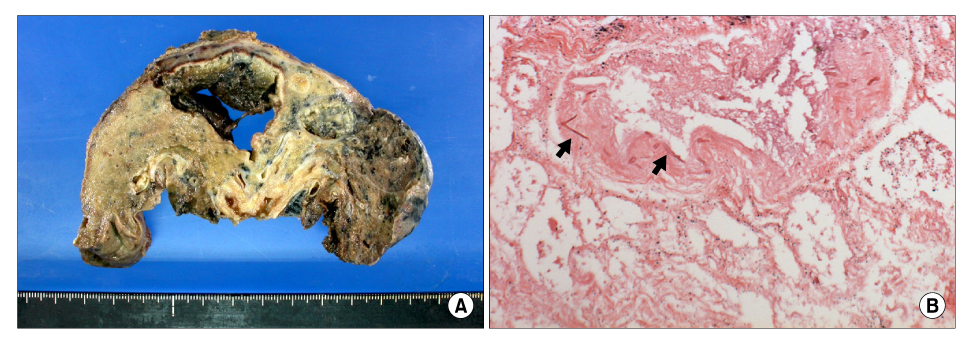
- Pulmonary mucormycosis is an uncommon, serious opportunistic infection caused by fungi belonging to the order Mucorales and it occurs exclusively in debilitated or immuno-compromised hosts. It is known that the fungi can invade the blood vessels and cause serious ischemic necrosis and bleeding5. We experienced a fatal case of pulmonary mucormycosis in a diabetic 75-year-old man who developed a progressive necrotizing lesion despite administering proper and prompt medical and surgical treatment. We report here on this case along with a review of the relevant medical literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Sugar AM. Mucormycosis. Clin Infect Dis. 1992. 14:S126–S129.2. Rinaldi MG. Zygomycosis. Infect Dis Clin North Am. 1989. 3:19–41.3. Virally ML, Riveline JP, Virally J, Chevojon P, Regnard JF, Belmekki A, et al. Pulmonay mucormycosis in a diabetic patient with HIV. Diabetes Care. 2002. 25:2105.4. Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999. 341:1906–1912.5. Davies SF, Knox KS, Sarosi GA. Mason RJ, Broaddus VC, Murray JF, Nadel JA, editors. Chapter 34. Fungal infection. Murray and Nadel's textbook of respiratory medicine. 2005. 4th ed. Philadelphia: Sanders Elsevier Inc;1073–1074. .6. Murray HW. Pulmonary mucormycosis with massive fatal hemoptysis. Chest. 1975. 68:65–68.7. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000. 13:236–301.8. Chang MS, Woo JH. Opportunistic fungal infection. Hanyang Med Rev. 2006. 26:20–33.9. McAdams HP, Rosado de Christenson M, Strollo DC, Patz EF Jr. Pulmonary mucormycosis: radiologic findings in 32 cases. AJR Am J Roentgenol. 1997. 168:1541–1548.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Pulmonary Mucormycosis: 1 case report
- A Case of Pulmonary Mucormycosis Presenting as an Endobronchial Mass
- Pulmonary mucormycosis with an appearance of consolidation
- Pulmonary mucormycosis presented as endobronchial lesion and a lobar consolidation in diabetes mellitus : A case report and review of other cases
- A Case of Pulmonary Mucormycosis without Obvious Predisposing Factors