Tuberc Respir Dis.
2006 Oct;61(4):356-365.
Significance of Corticosteroids and Their Relationship with Other Parameters in Patients with Sepsis
- Affiliations
-
- 1Department of Pulmonary and Critical care Medicine, Ajou University, School of Medicine, Suwon, Korea. parkkj@ajou.ac.kr
Abstract
-
BACKGROUND: Corticosteroids are known to be significant prognostic parameters in sepsis. Recently, an absolute and relative insufficiency of the corticosteroids system has often been reported to often develop particularly in severe sepsis. Degree of such an adrenal insufficiency not only has prognostic implications but also can be used to guide corticosteroids replacement therapy. The 24-hour urinary cortisol levels as well as serum cortisol concentrations were measured to assess the clinical significance and their relationship with the other parameters of sepsis, and also evaluated the clinical implications of the relative adrenal insufficiency.
METHODS
26 consecutive patients with sepsis were enrolled. The basal random serum cortisol, ACTH, ADH, lactate levels and 24-hour urinary free cortisol amount were measured. The rapid ACTH (250 microgram) stimulation test was also performed.
RESULTS
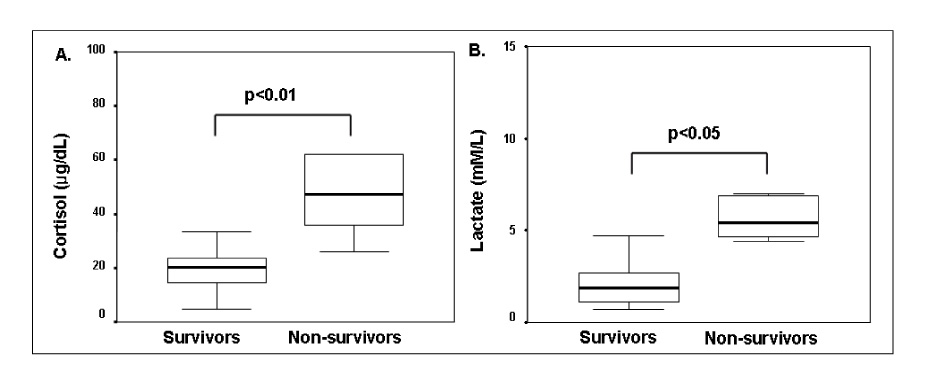
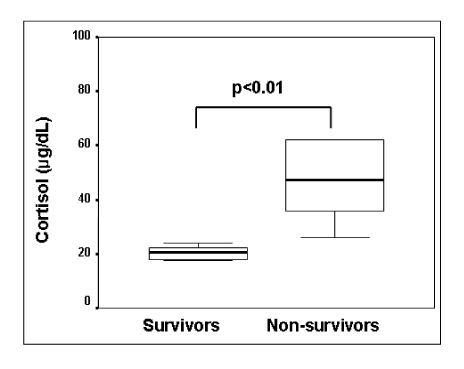
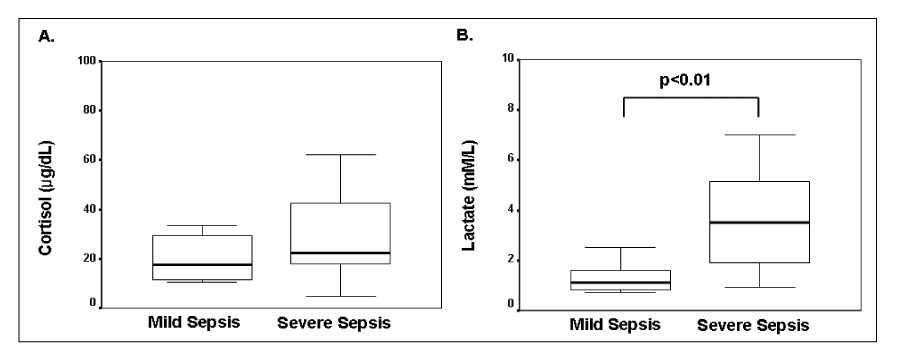
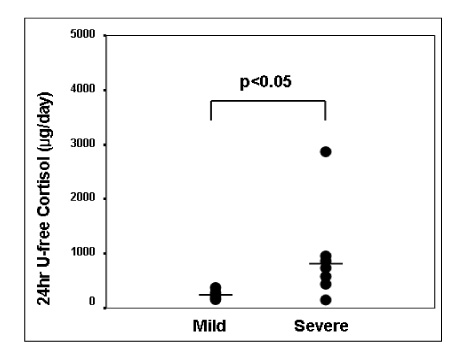
Basal serum cortisol levels were higher in the non-survivors than in the survivors. The 24-hour urinary free cortisol levels were higher in the patients with severe sepsis than in those without. The serum cortisol levels strongly correlated with the serum ADH and lactate levels. The 24-hour urinary free cortisol levels strongly correlated with the serum cortisol and lactate levels. The fractional changes in the cortisol levels after the rapid ACTH stimulation tests correlated with the serum cortisol, ADH, and lactate levels.
CONCLUSION
Both the serum cortisol and 24-hour urinary cortisol were found to be significant prognostic factors in sepsis, and showed a strong correlation with the other parameters. The relative adrenal insufficiency might also be an important clinical parameter.
MeSH Terms
Figure
Reference
-
1. Friedman G, Silva E, Vincent JL. Has the mortality of septic shock changed with time. Crit Care Med. 1998. 26:2078–2086.2. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002. 288:862–871.3. Lundberg JS, Perl TM, Wiblin T, Costigan MD, Dawson J, Nettleman MD, et al. Septic shock: an analysis of outcomes for patients with onset on hospital wards versus intensive care units. Crit Care Med. 1998. 26:1020–1024.4. Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J Psychosom Res. 2002. 53:865–871.5. El Azab SR, Rosseel PM, de Lange JJ, Groeneveld AB, van Strik R, van Wijk EM, et al. Dexamethasone decreases the pro- to anti-inflammatory cytokine ratio during cardiac surgery. Br J Anaesth. 2002. 88:496–501.6. Gonzalez H, Nardi O, Annane D. Relative adrenal failure in the ICU: an identifiable problem requiring treatment. Crit Care Clin. 2006. 22:105–118. vii.7. Barton RN, Stoner HB, Watson SM. Relationships among plasma cortisol, adrenocorticotrophin, and severity of injury in recently injured patients. J Trauma. 1987. 27:384–392.8. Chernow B, Alexander HR, Smallridge RC, Thompson WR, Cook D, Beardsley D, et al. Hormonal responses to graded surgical stress. Arch Intern Med. 1987. 147:1273–1278.9. Sam S, Corbridge TC, Mokhlesi B, Comellas AP, Molitch ME. Cortisol levels and mortality in severe sepsis. Clin Endocrinol. 2004. 60:29–35.10. Jarek MJ, Legare EJ, McDermott MT, Merenich JA, Kollef MH. Endocrine profiles for outcome prediction from the intensive care unit. Crit Care Med. 1993. 21:543–550.11. Drucker D, Shandling M. Variable adrenocortical function in acute medical illness. Crit Care Med. 1985. 13:477–479.12. Rothwell PM, Lawler PG. Prediction of outcome in intensive care patients using endocrine parameters. Crit Care Med. 1995. 23:78–83.13. McKee JI, Finlay WE. Cortisol replacement in severely stressed patients. Lancet. 1983. 1:484.14. Rothwell PM, Udwadia ZF, Lawler PG. Cortisol response to corticotropin and survival in septic shock. Lancet. 1991. 337:582–583.15. Bouachour G, Tirot P, Gouello JP, Mathieu E, Vincent JF, Alquier P. Adrenocortical function during septic shock. Intensive Care Med. 1995. 21:57–62.16. Burchard K. A review of the adrenal cortex and severe inflammation: quest of the "eucorticoid" state. J Trauma. 2001. 51:800–814.17. Bernard G. The International Sepsis Forum's controversies in sepsis: corticosteroids should not be routinely used to treat septic shock. Crit Care. 2002. 6:384–386.18. Soni A, Pepper GM, Wyrwinski PM, Ramirez NE, Simon R, Pina T, et al. Adrenal insufficiency occurring during septic shock: incidence, outcome, and relationship to peripheral cytokine levels. Am J Med. 1995. 98:266–271.19. Lamberts SW, Bruining HA, de Jong FH. Corticosteroid therapy in severe illness. N Engl J Med. 1997. 337:1285–1292.20. Meduri GU, Chrousos GP. Duration of glucocorticoid treatment and outcome in sepsis: is the right drug used the wrong way? Chest. 1998. 114:355–360.21. Prigent H, Maxime V, Annane D. Science review: mechanisms of impaired adrenal function in sepsis and molecular actions of glucocorticoids. Crit Care. 2004. 8:243–252.22. Moran JL, Chapman MJ, O'Fathartaigh MS, Peisach AR, Pannall PR, Leppard P. Hypocortisolaemia and adrenocortical responsiveness at onset of septic shock. Intensive Care Med. 1994. 20:489–495.23. Oppert M, Schindler R, Husung C, Offermann K, Graf KJ, Boenisch O, et al. Low-dose hydrocortisone improves shock reversal and reduces cytokine levels in early hyperdynamic septic shock. Crit Care Med. 2005. 33:2457–2464.24. Yildiz O, Doganay M, Aygen B, Guven M, Keleutimur F, Tutuu A. Physiological-dose steroid therapy in sepsis [ISRCTN36253388]. Crit Care. 2002. 6:251–259.25. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003. 29:530–538.26. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985. 13:818–829.27. Annane D, Sebille V, Troche G, Raphael JC, Gajdos P, Bellissant E. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000. 283:1038–1045.28. Venkatesh B, Mortimer RH, Couchman B, Hall J. Evaluation of random plasma cortisol and the low dose corticotropin test as indicators of adrenal secretory capacity in critically ill patients: a prospective study. Anaesth Intensive Care. 2005. 33:201–209.29. Loisa P, Uusaro A, Ruokonen E. A single adrenocorticotropic hormone stimulation test does not reveal adrenal insufficiency in septic shock. Anesth Analg. 2005. 101:1792–1798.30. Loisa P, Rinne T, Kaukinen S. Adrenocortical function and multiple organ failure in severe sepsis. Acta Anaesthesiol Scand. 2002. 46:145–151.31. Annane D, Bellissant E, Sebille V, Lesieur O, Mathieu B, Raphael JC, et al. Impaired pressor sensitivity to noradrenaline in septic shock patients with and without impaired adrenal function reserve. Br J Clin Pharmacol. 1998. 46:589–597.32. Esteban NV, Loughlin T, Yergey AL, Zawadzki JK, Booth JD, Winterer JC, et al. Daily cortisol production rate in man determined by stable isotope dilution/mass spectrometry. J Clin Endocrinol Metab. 1991. 72:39–45.33. Annane D, Sebille V, Bellissant E. Effect of low doses of corticosteroids in septic shock patients with or without early acute respiratory distress syndrome. Crit Care Med. 2006. 34:22–30.34. Smith I, Kumar P, Molloy S, Rhodes A, Newman PJ, Grounds RM, et al. Base excess and lactate as prognostic indicators for patients admitted to intensive care. Intensive Care Med. 2001. 27:74–83.35. Voerman HJ, Strack van Schijndel RJ, Groeneveld AB, de Boer H, Nauta JP, Thijs LG. Pulsatile hormone secretion during severe sepsis: accuracy of different blood sampling regimens. Metabolism. 1992. 41:934–940.36. Manglik S, Flores E, Lubarsky L, Fernandez F, Chhibber VL, Tayek JA. Glucocorticoid insufficiency in patients who present to the hospital with severe sepsis: a prospective clinical trial. Crit Care Med. 2003. 31:1668–1675.37. Rasmuson S, Olsson T, Hagg E. A low dose ACTH test to assess the function of the hypothalamicpituitary-adrenal axis. Clin Endocrinol. 1996. 44:151–156.38. Tordjman K, Jaffe A, Trostanetsky Y, Greenman Y, Limor R, Stern N. Low-dose (1 microgram) adrenocorticotrophin (ACTH) stimulation as a screening test for impaired hypothalamo-pituitary- adrenal axis function: sensitivity, specificity and accuracy in comparison with the high-dose (250 microgram) test. Clin Endocrinol. 2000. 52:633–640.39. Goodman S, Sprung CL, Ziegler D, Weiss YG. Cortisol changes among patients with septic shock and the relationship to ICU and hospital stay. Intensive Care Med. 2005. 31:1362–1369.40. Hamrahian AH, Oseni TS, Arafah BM. Measurements of serum free cortisol in critically ill patients. N Engl J Med. 2004. 350:1629–1638.41. Ho JT, Al-Musalhi H, Chapman MJ, Quach T, Thomas PD, Bagley CJ, et al. Septic shock and sepsis: a comparison of total and free plasma cortisol levels. J Clin Endocrinol Metab. 2006. 91:105–114.42. Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003. 31:1752–1758.43. Prigent H, Maxime V, Annane D. Clinical review: corticotherapy in sepsis. Crit Care. 2004. 8:122–129.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation of Nitric Oxide and Corticosteroids Along the Course of Sepsis
- Clinical Significance of serum Endothelin-1 and Interleukin-8 in Sepsis
- Mean cell volumes of neutrophils and monocytes are promising markers of sepsis in elderly patients
- The significance of sepsis severity score in multiple organ failure due to sepsis
- The significance of sepsis severity score in multiple organ failure due to sepsis