Tuberc Respir Dis.
2006 Jul;61(1):13-19.
Clinical Characteristics and Prognosis of Acinetobacter Nosocomial Pneumonia between MDR and non-MDR
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine of Hallym University Medical Center, Hallym University College of Medicine, Chuncheon, Korea. mglee@hallym.or.kr
Abstract
-
BACKGROUND: Acinetobacter baumannii has emerged as an important nosocomial pathogen worldwide. The incidence of these infections has recently begun to increase. The mortality rate associated with these infections is high (bacteremia; 52% , pneumonia: 23%~73%) and multidrug resistance has been reported. For the effective control of multidrug- resistant Acinetobacter baumannii(MDR-AB), the impact of these organisms in clinical practice should be determined. This study compared the clinical characteristics, mortality and morbidity of Acinetobacter nosocomial pneumonia between MDR strain and non-MDR strain.
METHODS
From Jan. 1, 2002 to Nov. 1. 2004, 47 adult patients with Acinetobacter nosocomial pneumonia in Chuncheon Sacred Heart Hospital were recruited and analyzed retrospectively. MDR-AB was defined as showing in vitro resistance to all commercially available antibiotics against A. baumannii.
RESULTS
There were 47 patients with Acinetobacter nosocomial pneumonia. MDR-AB and non MDR-AB was the cause of the pneumonia in 17 and 30 patients, respectively. Mean age of the former was 69+/-11 years old and the latter was 70+/-13 years old. The mean APCHE II score, ICU days and mortality were not different between the two groups(16.1+/-5.4 vs. 14.9+/-4.8, P=0.43, 25.1+/-13.6 vs. 39.1+/-31.0, P=0.2, 58.8% vs. 40%, P=0.21).
CONCLUSION
There are no significant differences in mortality and morbidity between MDR and non-MDR Acinetobacter baumannii. The mortality of the two groups is surprisingly high, therefore proper infection control practices are essential.
MeSH Terms
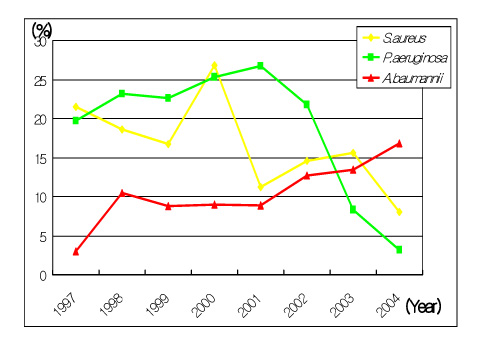
Figure
Reference
-
1. Allen DM, Hartman BJ. Mandell GL, Bennett JL, Dolin R, editors. Chapter 209. Acinetobacter species. Mandell, Douglas, and Bennett's principles and practice of infectious disease. 2000. 5th ed. Philadelphia: Churchill Livingstone;2339–2343.2. Bergogne-Berezin E. The increasing role of Acinetobacter species as nosocomial pathogens. Curr Infect Dis Rep. 2001. 3:440–444.3. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance(NNIS) report: data summary from October 1986-April 1996, issued May 1996. Am J infect Control. 1996. 24:380–388.4. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. Crit Care Med. 1999. 27:887–892.5. Bergogne-Berezin E. The increasing significance of outbreaks of Acinetobacter spp.: the need for control and new agents. J Hosp Infect. 1995. 30:Suppl. 441–452.6. Bergogne-Berezin E, Towner KJ. Acinetobacter spp. as nosocomial pathogens: microbial, clinical, and epidemiological features. Clin Microbiol Rev. 1996. 9:148–165.7. Getchell-White SI, Donowitz LG, Groschel DH. The inanimate environment of an intensive care unit as a potential source of nosocomial bacteria: evidence for long survival of Acinetobacter calcoaceticus. Infect Control Hosp Epidemiol. 1989. 10:402–407.8. Manikal VM, Landman D, Saurina G, Oydna E, Lal H, Quale J. Endemic carbapenem-resistant Acinetobacter species in Brooklyn, New York: citywide prevalence, interinstitutional spread, and relation to antibiotic usage. Clin Infect Dis. 2000. 31:101–106.9. el Shafie SS, Alishaq M, Leni Garcia M. Investigation of an outbreak of multidrug-resistant Acinetobacter baumannii in trauma intensive care unit. J Hosp Infect. 2004. 56:101–105.10. Acar JF. Consequences of bacterial resistance to antibiotics in medical practice. Clin Infect Dis. 1997. 24:Suppl. S17–S18.11. Ayan M, Durmaz R, Aktas E, Durmaz B. Bacteriological, clinical and epidemiological characteristics of hospital-acquired Acinetobacter baumannii infection in a teaching hospital. J Hosp Infect. 2003. 54:39–45.12. Landman D, Quale JM, Mayorga D, Adedeji A, Vangala K, Ravishankar J, et al. Citywide clonal outbreak of multiresistant Acinetobacter baumannii and Psuedomonas aeruginosa in Brooklyn, NY. Arch Intern Med. 2002. 162:1515–1520.13. Beck-Sague CM, Jarvis WR, Brook JH, Culver DH, Potts A, Gray E, et al. Epidemic bacteremia due to Acinetobacter baumannii in five intensive care units. Am J Epidemiol. 1990. 132:723–733.14. Seifert H, Strate A, Pulverer G. Nosocomial bacteremia due to Acinetobacter baumannii: clinical features, epidemiology, and predictors of mortality. Medicine. 1995. 74:340–349.15. Cisneros JM, Reyes MJ, Pachon J, Becerril B, Caballero FJ, Garcia-Garmendia JL, et al. Bacteremia due to Acinetobacter baumannii: epidemiology, clinical findings, and prognostic features. Clin Infect Dis. 1996. 22:1026–1032.16. Fagon JY, Chastre J, Domart Y, Trouillet JL, Gibert C. Mortality due to ventilator-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a proctected specimen brush. Clin Infect Dis. 1996. 23:538–542.17. Garcia-Garmendia JL, Ortiz-Leyba C, Garacho-Monero J, Jimenez-Jimenez FJ, Perez-Parede C, Barrero-Almodovar AE, et al. Risk factors for Acinetobacter baumannii nosocomial bacteremia in critically ill patients: a cohort study. Clin Infect Dis. 2001. 33:939–946.18. Go ES, Urban C, Burns J, Kreiswirth B, Eisner W, Mariano N, et al. Clinical and molecular epidemiology of Acinetobacter infections sensitive only to polymyxin B and sulbactam. Lancet. 1994. 344:1329–1332.19. Mahgoub S, Ahmed J, Glatt AE. Completely resistant Acinetobacter baummannii strains. Infect Control Hosp Epidemiol. 2002. 23:477–479.20. Simor AE, Lee M, Vearnocombe M, Jones-Paul L, Barry C, Gomez M, et al. An outbreak due to multiresistant Acinetobacter baumannii in a burn unit: risk factors for acquisition and management. Infect Control Hsop Epidemiol. 2002. 23:261–267.21. Wong TH, Tan BH, Ling ML, Song C. Multi-resistant Acinetobacter baumannii on a burn unit: clinical risk factors and prognosis. Burns. 2002. 28:349–357.22. Husni RN, Goldstein LS, Arroliga AC, Hall GS, Fatica C, Stoller JK, et al. Risk factors for an outbreak of Multidrug-resistant Acinetobacter nosocomial pneumonia among intubated patient. Chest. 1999. 115:1378–1382.23. Abbo A, Navon-Venezia S, Hammer-Muntz S, Krichali T, Siegaman-Igra Y, Carmeli Y. Multidrug-resistant Acinetobacter baumannii. Emerg Infect Dis. 2005. 11:22–29.24. Koeleman JG, Parleviest GA, Dijkshoorn L, Savelkoul PH, Vandengroucke-Grauls CM. Nosocomial outbreak of multi-resistant Acinetobacter baumannii on a surgical ward: epidemiology and risk factors for acquisition. J Hosp Infect. 1997. 37:113–123.25. Lortholary O, Fagon JY, Hoi AB, Slama MA, Pierre J, Giral P, et al. Nosocomial acquisition of multiresistant Acinetobacter baumannii: risk factors and prognosis. Clin Infect Dis. 1995. 20:790–796.26. Lee SO, Kim NJ, Choi SH, Kim TH, Chung JW, Woo JH, et al. Risk factors for acquisition of imipenem-resistant Acinetobacter baumnnii: a case-control study. Antimicrob Agents Chemother. 2004. 48:224–228.27. Husni RN, Goldstein LS, Arroliga AC, Hall GS, Fatica C, Stoller JK, et al. Risk factors for an outbreak of multidrug-resistant Acinetoacter nosocomial pneumonia among intubated patients. Chest. 1999. 115:1378–1382.28. Jain R, Danziger LH. Multidrug-resistant Acinetobacter infection: an emerging challenge to clinicians. Ann Pharmacother. 2004. 38:1449–1459.29. del Mar Tomas M, Cartelle M, Pertega S, Beceiro A, Linares P, Canle D, et al. Hospital outbreak caused by a carbapenem-resistant strain of Acinetobacter baumannii: patient prognosis and risk-factors for colonization and infection. Clin Microbiol Infect. 2005. 11:540–546.30. Lee SW, Jo HS, Kim WJ. Clinical characteristics of intensive care unit patients with carbapenem resistant Acinetobacter baumannii isolated from sputum. Tuberc Respir Dis. 2006. 60:228–234.. Mahanthanapak S, Chaiwarith R, Supparatpinyo K. Pan-drug resistant Acinetobacter baumannii at Maharaj Nakorn Chiang Mai Hospital. 2005. In : 5th International Symposium on Antimicrobial Agents and Resistance; –210. Abstract.32. Gomez J, Simarro E, Banos V, Requena L, Ruiz F, Garcia M, et al. Six-year prospective study of risk and progonositc factors in patients with nosocomial sepsis caused by Acinetobacter baumannii. Eur J Clin Microbiol Infect Dis. 1999. 18:358–361.33. Brun-Buisson C, Doyon F, Carlet J. Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. Am J Respir Crit Care Med. 1996. 154:617–624.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Community-Acquired Pneumonia Caused by Multidrug-Resistant Acinetobacter baumannii in Korea
- A Case of Multidrug-resistant Acinetobacter baumannii Ventriculitis Successfully Treated with Intrathecal Colistimethate
- A Trial of Aerosolized Colistin for the Treatment of Nosocomial Pneumonia due to Multidrug-resistant Acinetobacter baumannii
- Three Cases of Central Nervous System Infection Caused by Multi-Drug-Resistant Acinetobacter baumannii
- Effects of Aerosol Colistin Treatment of Pneumonia Caused by Multi-drug Resistant Acinetobacter baumannii