Korean J Urol.
2013 Feb;54(2):135-138.
Acute Epididymitis in Children: the Role of the Urine Test
- Affiliations
-
- 1Department of Urology, Yonsei University Wonju College of Medicine, Wonju, Korea. kkjksw@wonju.yonsei.ac.kr
Abstract
- PURPOSE
Acute epididymitis is considered to have an important role in children with scrotal pain. Recent reports have shown that urinalysis is not helpful for the diagnosis and treatment of acute epididymitis owing to negative microbiological findings. Therefore, we analyzed clinical and laboratory characteristics to examine the diagnostic yield of urinalysis in children.
MATERIALS AND METHODS
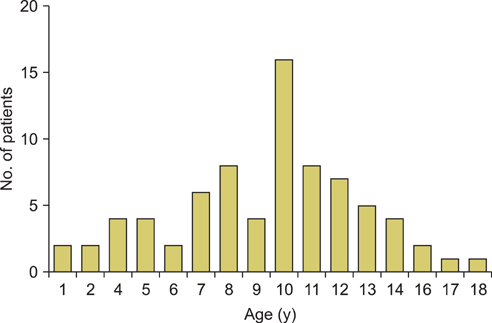
We retrospectively reviewed the medical records of 139 patients who were diagnosed with acute epididymitis from 2005 to 2011. Diagnosis was based on symptoms, physical findings, and color Doppler ultrasonography (DUS). To investigate the characteristics of epididymitis in children, the patients were divided into 3 groups: group A (aged less than 18 years, 76 patients), group B (18 to 35 years old, 19 patients), and group C (older than 35 years, 44 patients).
RESULTS
There were statistically significant differences in age, symptom duration, hospital stays, and lesion location in each group. White blood cell count and serum C-reactive protein levels, pyuria, and positive urine culture results were statistically higher in the older age group. The most common cause of acute epididymitis in children was idiopathic (96.1%).
CONCLUSIONS
In our group of children with epididymitis, 73 cases out of 76 (96.1%) resulted in negative pyuria in urinalysis. In addition, the most common cause of epididymitis was idiopathic. Because most urinalyses do not show pyuria, we believe that routine antibiotics may be not required in pediatric patients with epididymitis. If urinalysis shows pyuria with or without positive urine culture, antibiotics should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Somekh E, Gorenstein A, Serour F. Acute epididymitis in boys: evidence of a post-infectious etiology. J Urol. 2004. 171:391–394.2. McAndrew HF, Pemberton R, Kikiros CS, Gollow I. The incidence and investigation of acute scrotal problems in children. Pediatr Surg Int. 2002. 18:435–437.3. Santillanes G, Gausche-Hill M, Lewis RJ. Are antibiotics necessary for pediatric epididymitis? Pediatr Emerg Care. 2011. 27:174–178.4. Bukowski TP, Lewis AG, Reeves D, Wacksman J, Sheldon CA. Epididymitis in older boys: dysfunctional voiding as an etiology. J Urol. 1995. 154(2 Pt 2):762–765.5. Likitnukul S, McCracken GH Jr, Nelson JD, Votteler TP. Epididymitis in children and adolescents: a 20-year retrospective study. Am J Dis Child. 1987. 141:41–44.6. Gislason T, Noronha RF, Gregory JG. Acute epididymitis in boys: a 5-year retrospective study. J Urol. 1980. 124:533–534.7. Sakellaris GS, Charissis GC. Acute epididymitis in Greek children: a 3-year retrospective study. Eur J Pediatr. 2008. 167:765–769.8. Hutcheson J, Peters CA, Diamond DA. Amiodarone induced epididymitis in children. J Urol. 1998. 160:515–517.9. Kiviat MD, Shurtleff D, Ansell JS. Urinary reflux via the vas deferens: unusual cause of epididymitis in infancy. J Pediatr. 1972. 80:476–479.10. Berger RE. Acute epididymitis. Sex Transm Dis. 1981. 8:286–289.11. Takahashi S, Kurimura Y, Hashimoto J, Sunaoshi K, Takeda K, Suzuki N, et al. Management for males whose female partners are diagnosed with genital chlamydial infection. J Infect Chemother. 2011. 17:76–79.12. Ito S, Tsuchiya T, Yasuda M, Yokoi S, Nakano M, Deguchi T. Prevalence of genital mycoplasmas and ureaplasmas in men younger than 40 years-of-age with acute epididymitis. Int J Urol. 2012. 19:234–238.13. Haecker FM, Hauri-Hohl A, von Schweinitz D. Acute epididymitis in children: a 4-year retrospective study. Eur J Pediatr Surg. 2005. 15:180–186.14. Park CH, Im JK, Kim KK, Park HW. Clinical characteristics of acute epididymitis in children and adults. Korean J Urol. 1999. 40:674–676.15. van Gool JD, Hjalmas K, Tamminen-Mobius T, Olbing H. Historical clues to the complex of dysfunctional voiding, urinary tract infection and vesicoureteral reflux. The International Reflux Study in Children. J Urol. 1992. 148(5 Pt 2):1699–1702.16. Al-Taheini KM, Pike J, Leonard M. Acute epididymitis in children: the role of radiologic studies. Urology. 2008. 71:826–829.17. Kim JM, Lee CY, Lee SD. Acute epididymitis in children; 10-year retrospective study of single center. Korean J Urogenit Tract Infect Inflamm. 2007. 2:173–178.18. Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008. 35:101–108.19. Graumann LA, Dietz HG, Stehr M. Urinalysis in children with epididymitis. Eur J Pediatr Surg. 2010. 20:247–249.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics of Acute Epididymitis in Children and Adults
- Clinical Characteristics of Acute Epididymitis in Prepubertal Patients
- Early exploration of acute scrotum in children
- The Relationship between Clinical Symptoms and Urine Culture in Adult Patients with Acute Epididymitis
- Clinical observation of 30 cases who underwent epididymectomy: especially, on the cases of tuberculous epididymitis