Korean J Urol.
2012 Feb;53(2):92-97.
Efficacy of Alpha Blocker Treatment According to the Degree of Intravesical Prostatic Protrusion Detected by Transrectal Ultrasonography in Patients with Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, Hanyang University College of Medicine, Seoul, Korea. moonuro@hanyang.ac.kr
Abstract
- PURPOSE
To analyze the effectiveness of tamsulosin 0.2 mg once daily for 3 months according to the degree of intravesical prostatic protrusion (IPP) in patients with benign prostatic hyperplasia (BPH).
MATERIALS AND METHODS
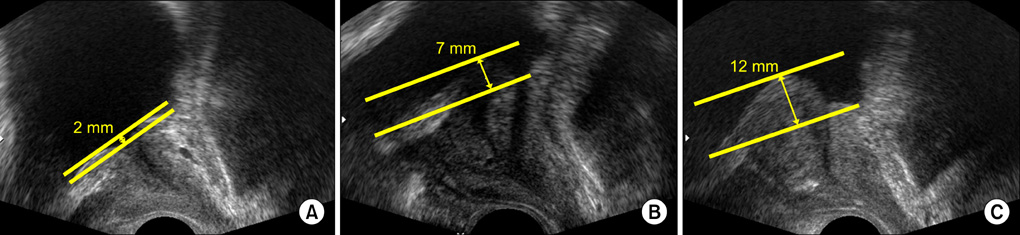
A total of 134 BPH patients over 40 years of age treated with tamsulosin 0.2 mg between January 2007 and January 2009 were enrolled retrospectively. The patients were classified into three groups according to the degree of IPP: below 5 mm (group A), between 5 and 10 mm (group B), and over 10 mm (group C). Prostate volume, prostate-specific antigen (PSA), prostatic urethral length (PUL), and prostatic adenoma urethral length (PAUL) were evaluated before treatment. International Prostate Symptom Score and Quality of Life (IPSS/QoL), maximal urine flow rate (Qmax), and postvoid residual (PVR) volume were measured before treatment, and improvement in the three groups was compared after 3 months.
RESULTS
The mean age of the patients was 65.01+/-7.38 years. Mean IPPs were 0.90+/-1.39 mm (group A, n=90), 6.92+/-1.10 mm (group B, n=24), and 16.60+/-4.06 mm (group C, n=20). Prostate volume, PUL, PAUL, PSA, Qmax, and PVR showed significant correlations with IPP (p<0.05), but not with IPSS/QoL score (p>0.05). Comparison of parameters before and after 3 months showed that medication improved total IPSS and subscores (p<0.001), QoL (p<0.001), Qmax (p<0.001), and PVR (p=0.030) in group A. In group B, it improved total IPSS (p=0.01), irritative subscore (p<0.001), and obstructive subscore (p=0.03). In group C, only total IPSS (p=0.01) and irritative score (p<0.001) were significantly improved.
CONCLUSIONS
Tamsulosin may be more effective in improving symptom scores and Qmax in patients with mild IPP than in those with moderate or severe IPP.
Keyword
MeSH Terms
Figure
Reference
-
1. Chute CG, Panser LA, Girman CJ, Oesterling JE, Guess HA, Jacobsen SJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993. 150:85–89.2. Lim KB, Ho H, Foo KT, Wong MY, Fook-Chong S. Comparison of intravesical prostatic protrusion, prostate volume and serum prostatic-specific antigen in the evaluation of bladder outlet obstruction. Int J Urol. 2006. 13:1509–1513.3. Reis LO, Barreiro GC, Baracat J, Prudente A, D'Ancona CA. Intravesical protrusion of the prostate as a predictive method of bladder outlet obstruction. Int Braz J Urol. 2008. 34:627–633.4. Kim BH, Sohn JC, Park CH, Kim CI. The usefulness of intravesical prostatic protrusion and bladder wall thickness measurement using transabdominal ultrasound in patients with benign prostatic hyperplasia. Korean J Urol. 2005. 46:1180–1185.5. Nose H, Foo KT, Lim KB, Yokoyama T, Ozawa H, Kumon H. Accuracy of two noninvasive methods of diagnosing bladder outlet obstruction using ultrasonography: intravesical prostatic protrusion and velocity-flow video urodynamics. Urology. 2005. 65:493–497.6. Lee JM, Chung H, Kim TW, Kim HS, Wang JH, Yang SK. The correlation of intravesical prostatic protrusion with storage symptoms, as measured by transrectal ultrasound. Korean J Urol. 2008. 49:145–149.7. Doo CK, Uh HS. Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology. 2009. 73:232–236.8. John H, Hauri D, Bangerter U, Elbadawi A. Ultrastructure of the trigone and its functional implications. Urol Int. 2001. 67:264–271.9. Kuo HC. Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology. 1999. 54:90–96.10. Lee SW, Cho JM, Kang JY, Yoo TK. Clinical and urodynamic significance of morphological differences in intravesical prostatic protrusion. Korean J Urol. 2010. 51:694–699.11. Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003. 91:371–374.12. Arnolds M, Oelke M. Positioning invasive versus noninvasive urodynamics in the assessment of bladder outlet obstruction. Curr Opin Urol. 2009. 19:55–62.13. Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004. 46:547–554.14. Franco G, De Nunzio C, Leonardo C, Tubaro A, Ciccariello M, De Dominicis C, et al. Ultrasound assessment of intravesical prostatic protrusion and detrusor wall thickness--new standards for noninvasive bladder outlet obstruction diagnosis? J Urol. 2010. 183:2270–2274.15. Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology. 2007. 70:1096–1099.16. Kim KH, Kim YS. Correlation of male overactive bladder with intravesical prostatic protrusion. Korean J Urol. 2010. 51:843–846.17. Lee LS, Sim HG, Lim KB, Wang D, Foo KT. Intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. Int J Urol. 2010. 17:69–74.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging of tbe Prostatic Carcinoma and Benign Prostatic Hyperplasia by Transrectal Ultrasound
- The Effect of alpha-Blocker Treatment for Nocturia with Benign Prostatic Hyperplasia
- The Efficacy of the Alpha-Blocker, Tamsulosin, in the Patients with Benign Prostatic Hyperplasia of 30 grams or less
- Diagnostic Value of Transrectal Ultrasonography for Prostatic Cancer
- Effect Of Alpha: Adrenergic Blocker In Thermoresistant Benign Prostatic Hyperplasia