Korean J Urol.
2012 Feb;53(2):69-77.
Chronic Prostatitis: Approaches for Best Management
- Affiliations
-
- 1Department of Urology, Dongguk University School of Medicine, Gyeongju, Korea. ksleemd@dongguk.ac.kr
Abstract
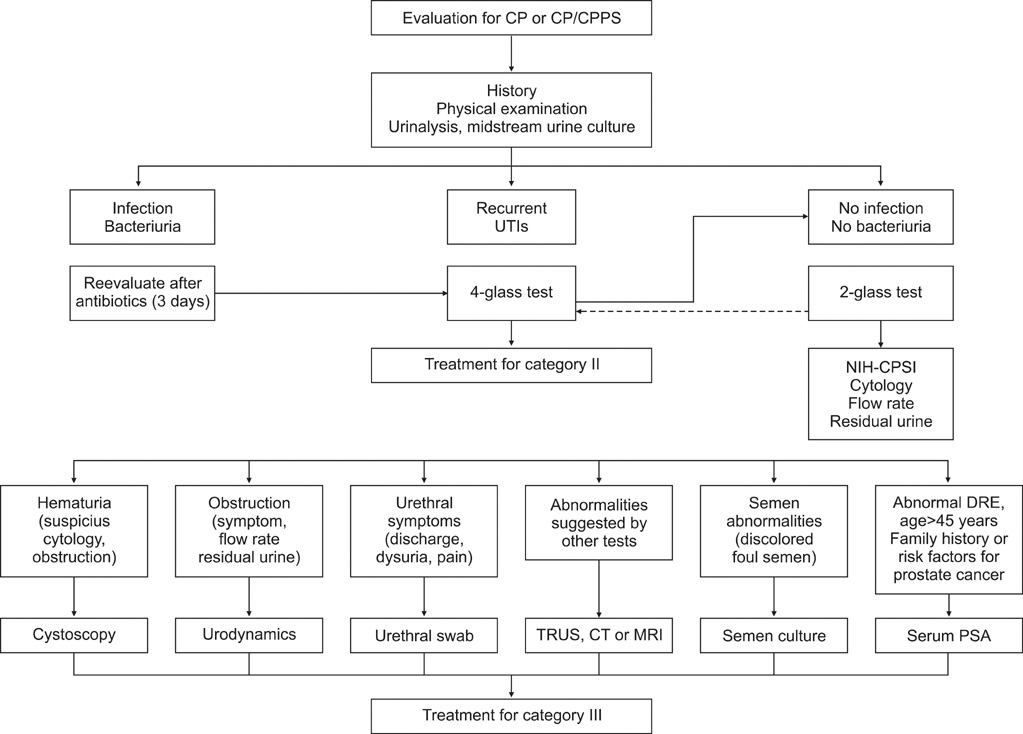
- Prostatitis is a prevalent condition that encompasses a large array of clinical symptoms with significant impacts on men's life. The diagnosis and treatment of this disorder presents numerous challenges for urologists, most notably, a lack of specific and effective diagnostic methods. Chronic bacterial prostatitis is successfully treated with appropriate antibiotics that penetrate the prostate and kill the causative organisms. Prostatitis category III (chronic pelvic pain syndrome) is common, very bothersome, and enigmatic. Symptoms are usually prolonged and, generally speaking, treatment results are unsatisfactory. During the last decade, research has focused on the distress caused by the condition, but although our knowledge has certainly increased, there have been no real breakthroughs; controversies and many unanswered questions remain. Furthermore, the optimal management of category III prostatitis is not known. Conventional prolonged courses of antibiotic therapy have not proven to be efficacious. Novel therapies providing some evidence for efficacy include alpha-blocker, anti-inflammatory phytotherapy, physiotherapy, neuroleptics, and others, each offering therapeutic mechanisms. A stepwise approach involving multimodal therapy is often successful for treating patients. The UPOINT technique has been used to clinically phenotype these patients and drive the appropriate selection of multimodal therapy.
MeSH Terms
Figure
Reference
-
1. Krieger JN, Riley DE, Cheah PY, Liong ML, Yuen KH. Epidemiology of prostatitis: new evidence for a world-wide problem. World J Urol. 2003. 21:70–74.2. Yoo YN. Prostatitis. Korean J Urol. 1994. 35:575–585.3. McNaughton Collins M, Pontari MA, O'Leary MP, Calhoun EA, Santanna J, Landis JR, et al. Quality of life is impaired in men with chronic prostatitis: the Chronic Prostatitis Collaborative Research Network. J Gen Intern Med. 2001. 16:656–662.4. Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001. 165:842–845.5. Nickel JC, Nigro M, Valiquette L, Anderson P, Patrick A, Mahoney J, et al. Diagnosis and treatment of prostatitis in Canada. Urology. 1998. 52:797–802.6. Kiyota H, Onodera S, Ohishi Y, Tsukamoto T, Matsumoto T. Questionnaire survey of Japanese urologists concerning the diagnosis and treatment of chronic prostatitis and chronic pelvic pain syndrome. Int J Urol. 2003. 10:636–642.7. Pontari MA, Joyce GF, Wise M, McNaughton-Collins M. Prostatitis. J Urol. 2007. 177:2050–2057.8. Nickel JC, Olson ME, Costerton JW. Rat model of experimental bacterial prostatitis. Infection. 1991. 19:Suppl 3. S126–S130.9. Schaeffer AJ, Landis JR, Knauss JS, Propert KJ, Alexander RB, Litwin MS, et al. Demographic and clinical characteristics of men with chronic prostatitis: the national institutes of health chronic prostatitis cohort study. J Urol. 2002. 168:593–598.10. de la Rosette JJ, Hubregtse MR, Karthaus HF, Debruyne FM. Results of a questionnaire among Dutch urologists and general practitioners concerning diagnostics and treatment of patients with prostatitis syndromes. Eur Urol. 1992. 22:14–19.11. Moon TD. Questionnaire survey of urologists and primary care physicians' diagnostic and treatment practices for prostatitis. Urology. 1997. 50:543–547.12. Yang J, Liu L, Xie HW, Ginsberg DA. Chinese urologists' practice patterns of diagnosing and treating chronic prostatitis: a questionnaire survey. Urology. 2008. 72:548–551.13. Krieger JN, Riley DE. Chronic prostatitis: Charlottesville to Seattle. J Urol. 2004. 172:2557–2560.14. Ku JH, Paick JS, Kim SW. Chronic prostatitis in Korea: a nationwide postal survey of practicing urologists in 2004. Asian J Androl. 2005. 7:427–432.15. Mehik A, Hellstrom P, Sarpola A, Lukkarinen O, Jarvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001. 88:35–38.16. Nickel JC. The biomedical model has failed! So what is next. Contemp Urol. 2006. 1:31–39.17. Yang CC, Lee JC, Kromm BG, Ciol MA, Berger RE. Pain sensitization in male chronic pelvic pain syndrome: why are symptoms so difficult to treat? J Urol. 2003. 170:823–826.18. Kirby RS, Lowe D, Bultitude MI, Shuttleworth KE. Intra-prostatic urinary reflux: an aetiological factor in abacterial prostatitis. Br J Urol. 1982. 54:729–731.19. Persson BE, Ronquist G. Evidence for a mechanistic association between nonbacterial prostatitis and levels of urate and creatinine in expressed prostatic secretion. J Urol. 1996. 155:958–960.20. Staud R. Fibromyalgia pain: do we know the source? Curr Opin Rheumatol. 2004. 16:157–163.21. Dadabhoy D, Clauw DJ. Fibromyalgia: progress in diagnosis and treatment. Curr Pain Headache Rep. 2005. 9:399–404.22. Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders--pathways of vulnerability. Pain. 2006. 123:226–230.23. Yilmaz U, Liu YW, Berger RE, Yang CC. Autonomic nervous system changes in men with chronic pelvic pain syndrome. J Urol. 2007. 177:2170–2174.24. McNaughton Collins M, MacDonald R, Wilt TJ. Diagnosis and treatment of chronic abacterial prostatitis: a systematic review. Ann Intern Med. 2000. 133:367–381.25. Nickel JC. Classification and diagnosis of prostatitis: a gold standard? Andrologia. 2003. 35:160–167.26. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol. 1999. 162:369–375.27. Roberts RO, Jacobson DJ, Girman CJ, Rhodes T, Lieber MM, Jacobsen SJ. Low agreement between previous physician diagnosed prostatitis and national institutes of health chronic prostatitis symptom index pain measures. J Urol. 2004. 171:279–283.28. Schneider H, Wilbrandt K, Ludwig M, Beutel M, Weidner W. Prostate-related pain in patients with chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2005. 95:238–243.29. Nickel JC, Shoskes D, Wang Y, Alexander RB, Fowler JE Jr, Zeitlin S, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006. 176:119–124.30. Weidner W, Anderson RU. Evaluation of acute and chronic bacterial prostatitis and diagnostic management of chronic prostatitis/chronic pelvic pain syndrome with special reference to infection/inflammation. Int J Antimicrob Agents. 2008. 31:Suppl 1. S91–S95.31. Schaeffer AJ, Knauss JS, Landis JR, Propert KJ, Alexander RB, Litwin MS, et al. Leukocyte and bacterial counts do not correlate with severity of symptoms in men with chronic prostatitis: the National Institutes of Health Chronic Prostatitis Cohort Study. J Urol. 2002. 168:1048–1053.32. Kaplan SA, Te AE, Jacobs BZ. Urodynamic evidence of vesical neck obstruction in men with misdiagnosed chronic nonbacterial prostatitis and the therapeutic role of endoscopic incision of the bladder neck. J Urol. 1994. 152:2063–2065.33. Kaplan SA, Santarosa RP, D'Alisera PM, Fay BJ, Ikeguchi EF, Hendricks J, et al. Pseudodyssynergia (contraction of the external sphincter during voiding) misdiagnosed as chronic nonbacterial prostatitis and the role of biofeedback as a therapeutic option. J Urol. 1997. 157:2234–2237.34. Weidner W, Ludwig M, Brahler E, Schiefer HG. Outcome of antibiotic therapy with ciprofloxacin in chronic bacterial prostatitis. Drugs. 1999. 58:Suppl 2. 103–106.35. Schaeffer AJ, Anderson RU, Krieger JN, Lobel B, Naber K, Nakagawa M. McConnel J, Abrams P, Denis L, editors. The assessment and management of male pelvic pain syndrome including prostatitis. Male lower urinary tract dysfunction evaluation and management; 6th International Consultation on New Developments in Prostate Cancer and Prostate Diseases. 2006. Paris: Health Publications;341–385.36. Cho IR, Keener TS, Nghiem HV, Winter T, Krieger JN. Prostate blood flow characteristics in the chronic prostatitis/pelvic pain syndrome. J Urol. 2000. 163:1130–1133.37. Nadler RB, Collins MM, Propert KJ, Mikolajczyk SD, Knauss JS, Landis JR, et al. Prostate-specific antigen test in diagnostic evaluation of chronic prostatitis/chronic pelvic pain syndrome. Urology. 2006. 67:337–342.38. Pavone-Macaluso M. Chronic prostatitis syndrome: a common, but poorly understood condition. Part I. EAU-EBU Update Series. 2007. 5:1–15.39. Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009. 73:538–542.40. Frazier HA, Spalding TH, Paulson DF. Total prostatoseminal vesiculectomy in the treatment of debilitating perineal pain. J Urol. 1992. 148:409–411.41. Mo KI, Lee KS, Kim DG. Efficacy of combination therapy for patients with chronic prostatitis/chronic pelvic pain syndrome: a prospective study. Korean J Urol. 2006. 47:536–540.42. Cheah PY, Liong ML, Yuen KH, Teh CL, Khor T, Yang JR, et al. Terazosin therapy for chronic prostatitis/chronic pelvic pain syndrome: a randomized, placebo controlled trial. J Urol. 2003. 169:592–596.43. Mehik A, Alas P, Nickel JC, Sarpola A, Helstrom PJ. Alfuzosin treatment for chronic prostatitis/chronic pelvic pain syndrome: a prospective, randomized, double-blind, placebo-controlled, pilot study. Urology. 2003. 62:425–429.44. Evliyaoglu Y, Burgut R. Lower urinary tract symptoms, pain and quality of life assessment in chronic non-bacterial prostatitis patients treated with alpha-blocking agent doxazosin; versus placebo. Int Urol Nephrol. 2002. 34:351–356.45. Nickel JC, Narayan P, McKay J, Doyle C. Treatment of chronic prostatitis/chronic pelvic pain syndrome with tamsulosin: a randomized double blind trial. J Urol. 2004. 171:1594–1597.46. Yang G, Wei Q, Li H, Yang Y, Zhang S, Dong Q. The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials. J Androl. 2006. 27:847–852.47. Nickel JC, Krieger JN, McNaughton-Collins M, Anderson RU, Pontari M, Shoskes DA, et al. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. N Engl J Med. 2008. 359:2663–2673.48. Chuang YC, Yoshimura N, Wu M, Huang CC, Chiang PH, Tyagi P, et al. Intraprostatic capsaicin injection as a novel model for nonbacterial prostatitis and effects of botulinum toxin A. Eur Urol. 2007. 51:1119–1127.49. Bach D, Walker H. How important are prostaglandins in the urology of man? Urol Int. 1982. 37:160–171.50. Nickel JC, Forrest JB, Tomera K, Hernandez-Graulau J, Moon TD, Schaeffer AJ, et al. Pentosan polysulfate sodium therapy for men with chronic pelvic pain syndrome: a multicenter, randomized, placebo controlled study. J Urol. 2005. 173:1252–1255.51. Smith KB, Tripp D, Pukall C, Nickel JC. Predictors of sexual and relationship functioning in couples with Chronic Prostatitis/Chronic pelvic pain syndrome. J Sex Med. 2007. 4:734–744.52. Cornel EB, van Haarst EP, Schaarsberg RW, Geels J. The effect of biofeedback physical therapy in men with chronic pelvic pain syndrome type III. Eur Urol. 2005. 47:607–611.53. Anderson RU, Wise D, Sawyer T, Chan C. Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men. J Urol. 2005. 174:155–160.54. Holroyd KA, O'Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, Carlson BW. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA. 2001. 285:2208–2215.55. Shoskes DA, Hakim L, Ghoniem G, Jackson CL. Long-term results of multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2003. 169:1406–1410.56. Tugcu V, Tasci AI, Fazlioglu A, Gurbuz G, Ozbek E, Sahin S, et al. A placebo-controlled comparison of the efficiency of triple- and monotherapy in category III B chronic pelvic pain syndrome (CPPS). Eur Urol. 2007. 51:1113–1117. discussion 8.57. Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009. 12:177–183.58. Shoskes DA, Nickel JC, Kattan MW. Phenotypically directed multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome: a prospective study using UPOINT. Urology. 2010. 75:1249–1253.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Concentrations of Zinc in Expressed Prostatic Secretion of Chronic Prostatitis Patients
- Clinical Effects of Serenoa Repens(Permixon) on Chronic Prostatitis
- Clinical Evaluation of Cernilton in Chronic Prostatitis
- Chronic Prostatitis and Urethritis
- A Symptomatic Study of Depressive Phenomena on Chronic Prostatitis