Korean J Urol.
2012 Apr;53(4):234-239.
Discontinuation of Anticoagulant or Antiplatelet Therapy for Transrectal Ultrasound-Guided Prostate Biopsies: A Single-Center Experience
- Affiliations
-
- 1Department of Urology, St James's Hospital, Dublin, Ireland. omerraheem@gmail.com
Abstract
- PURPOSE
Historically, it was thought that hemorrhagic complications were increased with transrectal ultrasound-guided prostate biopsies (TRUS biopsy) of patients receiving anticoagulation/antiplatelet therapy. However, the current literature supports the continuation of anticoagulation/antiplatelet therapy without additional morbidity. We assessed our experience regarding the continuation of anticoagulation/antiplatelet therapy during TRUS biopsy.
MATERIALS AND METHODS
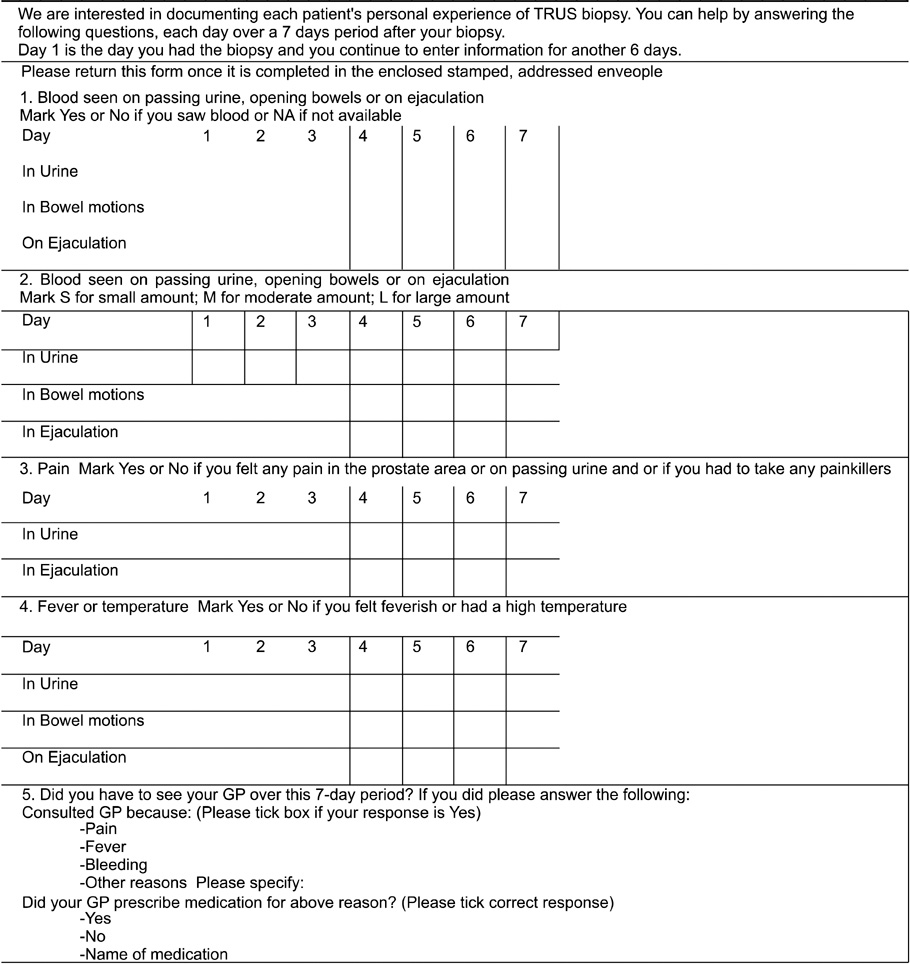
A total of 91 and 98 patients were included in the anticoagulation/antiplatelet (group I) and control (group II) groups, respectively. Group I subgroups consisted of patients on monotherapy or dual therapy of aspirin, warfarin, clopidogrel, or low molecular weight heparin. The TRUS biopsy technique was standardized to 12 cores from the peripheral zones. Patients completed a questionnaire over the 7 days following TRUS biopsy. The questionnaire was designed to assess the presence of hematuria, rectal bleeding, and hematospermia. Development of rectal pain, fever, and emergency hospital admissions following TRUS biopsy were also recorded.
RESULTS
The patients' mean age was 65 years (range, 52 to 74 years) and 63.5 years (range, 54 to 74 years) in groups I and II, respectively. The overall incidence of hematuria was 46% in group I compared with 63% in group II (p=0.018). The incidence of hematospermia was 6% and 10% in groups I and II, respectively. The incidence of rectal bleeding was similar in group I (40%) and group II (39%). Statistical analysis was conducted by using Fisher exact test.
CONCLUSIONS
There were fewer hematuria episodes in anticoagulation/antiplatelet patients. This study suggests that it is not necessary to discontinue anticoagulation/antiplatelet treatment before TRUS biopsy.
MeSH Terms
Figure
Reference
-
1. Ghani KR, Dundas D, Patel U. Bleeding after transrectal ultrasonography-guided prostate biopsy: a study of 7-day morbidity after a six-, eight- and 12-core biopsy protocol. BJU Int. 2004. 94:1014–1020.2. Raaijmakers R, Kirkels WJ, Roobol MJ, Wildhagen MF, Schrder FH. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002. 60:826–830.3. Burger W, Chemnitius JM, Kneissl GD, Rücker G. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis. J Intern Med. 2005. 257:399–414.4. Travis S, Wray R, Harrison K. Perioperative anticoagulant control. Br J Surg. 1989. 76:1107–1108.5. Connor SE, Wingate JP. Management of patients treated with aspirin or warfarin and evaluation of haemostasis prior to prostatic biopsy: a survey of current practice amongst radiologists and urologists. Clin Radiol. 1999. 54:598–603.6. Nambirajan T, Woolsey S, Mahendra V, Walsh IK, Lynch TH, Keane PF. Efficacy and safety peri-prostatic local anaesthetic injection in trans-rectal biopsy of the prostrate: a prospective randomised study. Surgeon. 2004. 2:221–224.7. Douketis JD, Berger PB, Dunn AS, Jaffer AK, Spyropoulos AC, Becker RC, et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 299S–339S.8. Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol. 2003. 41:159–168.9. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, King SB 3rd, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention). Circulation. 2006. 113:e166–e286.10. Mehta SR, Yusuf S, Peters RJ, Bertrand ME, Lewis BS, Natarajan MK, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001. 358:527–533.11. Steinhubl SR, Berger PB, Mann JT 3rd, Fry ET, DeLago A, Wilmer C, et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002. 288:2411–2420.12. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006. 119:624–638.13. Chassot PG, Delabays A, Spahn DR. Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth. 2007. 99:316–328.14. Pickard AS, Becker RC, Schumock GT, Frye CB. Clopidogrel-associated bleeding and related complications in patients undergoing coronary artery bypass grafting. Pharmacotherapy. 2008. 28:376–392.15. Pass SE, Simpson RW. Discontinuation and reinstitution of medications during the perioperative period. Am J Health Syst Pharm. 2004. 61:899–912.16. Dunning J, Versteegh M, Fabbri A, Pavie A, Kolh P, Lockowandt U, et al. Guideline on antiplatelet and anticoagulation management in cardiac surgery. Eur J Cardiothorac Surg. 2008. 34:73–92.17. Cahill RA, McGreal GT, Crowe BH, Ryan DA, Manning BJ, Cahill MR, et al. Duration of increased bleeding tendency after cessation of aspirin therapy. J Am Coll Surg. 2005. 200:564–573.18. Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003. 290:2685–2692.19. Mukerji G, Munasinghe I, Raza A. A survey of the peri-operative management of urological patients on clopidogrel. Ann R Coll Surg Engl. 2009. 91:313–320.20. Palan J, Odutola A, White SP. Is clopidogrel stopped prior to hip fracture surgery--A survey of current practice in the United Kingdom. Injury. 2007. 38:1279–1285.21. Maan Z, Cutting CW, Patel U, Kerry S, Pietrzak P, Perry MJ, et al. Morbidity of transrectal ultrasonography-guided prostate biopsies in patients after the continued use of low-dose aspirin. BJU Int. 2003. 91:798–800.22. Halliwell OT, Yadegafar G, Lane C, Dewbury KC. Transrectal ultrasound-guided biopsy of the prostate: aspirin increases the incidence of minor bleeding complications. Clin Radiol. 2008. 63:557–561.23. Giannarini G, Mogorovich A, Valent F, Morelli G, De Maria M, Manassero F, et al. Continuing or discontinuing low-dose aspirin before transrectal prostate biopsy: results of a prospective randomized trial. Urology. 2007. 70:501–505.24. Ihezue CU, Smart J, Dewbury KC, Mehta R, Burgess L. Biopsy of the prostate guided by transrectal ultrasound: relation between warfarin use and incidence of bleeding complications. Clin Radiol. 2005. 60:459–463.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pain during Transrectal Ultrasound-Guided Prostate Biopsy and the Role of Periprostatic Nerve Block: What Radiologists Should Know
- Prostate Cancer Detection by Transrectal Ultrasound Guided Prostate Biopsy: Urology versus Radiology at a Single Academic Institution
- Value of Hypoechoic Lesions in the Diagnosis of Prostate Cancer with Transrectai Ultrasonographically Guided Biopsies
- The Criteria for the Decision of Transrectal US-Guided Prostate Biopsy: Can We Reduce the Number of Unnecessary Biopsies?
- Effect of Periprostatic Nerve Blockade for Transrectal Ultrasound Guided Biopsy of the Prostate