Lab Med Online.
2011 Jul;1(3):153-157.
Re-evaluation of the Anti-streptolysin O Test for Systemic Rheumatic Diseases
- Affiliations
-
- 1Department of Laboratory Medicine, College of Medicine, Hanyang University, Seoul, Korea. tykim@hanyang.ac.kr
Abstract
- BACKGROUND
Anti-streptolysin O (ASO) test is usually used to diagnose group A streptococcal infection-related diseases, such as rheumatic fever, reactive arthritis, and various infectious diseases. Despite the recent declining incidence of these diseases, ASO test is still frequently performed as a screening test to diagnose rheumatic diseases. This study re-evaluated the clinical usefulness of ASO test in systemic rheumatic diseases (SRD).
METHODS
ASO tests was performed in 825 patients between April and October in 2010. ASO levels were compared between SRD and non-SRD groups of patients. The results of ASO, C-reactive protein (CRP), and rheumatoid factor (RF) were compared among 6 subgroups of SRD: rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, Behcet disease, Sjogren's syndrome and others.
RESULTS
Positive results in ASO test (>200 IU/mL) were observed in 15.3% (126/825) of the patients tested. None of the ASO positive patients was, however, diagnosed with rheumatic fever or reactive arthritis. There were no statistically significant differences in the mean value (P=0.688) or positive rate (P=0.835) of ASO test between SRD and non-SRD groups. Positive rates of ASO test were also not statistically significant different among six subgroups of SRD patients (all P>0.05), whereas those of CRP and RF tests were significantly different.
CONCLUSIONS
The usefulness of ASO test is very low for diagnosing SRD, although it is frequently carried out as a screening test. We suggest that ASO test must be performed selectively when diseases from group A streptococcal infection are suspected.
MeSH Terms
-
Arthritis, Reactive
Arthritis, Rheumatoid
Behcet Syndrome
C-Reactive Protein
Communicable Diseases
Humans
Incidence
Lupus Erythematosus, Systemic
Mass Screening
Rheumatic Diseases
Rheumatic Fever
Rheumatoid Factor
Sjogren's Syndrome
Spondylitis, Ankylosing
Streptococcal Infections
C-Reactive Protein
Rheumatoid Factor
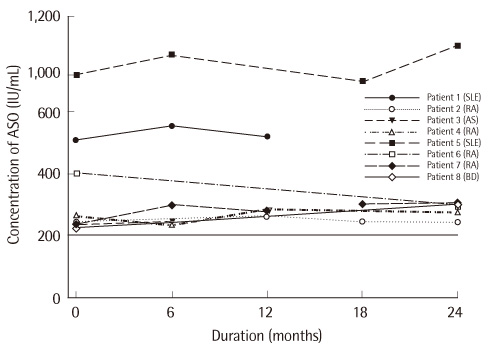
Figure
Reference
-
1. Shulman ST, Tanz RR. Group A streptococcal pharyngitis and immune-mediated complications: from diagnosis to management. Expert Rev Anti Infect Ther. 2010. 8:137–150.
Article2. Carapetis JR, McDonald M, Wilson NJ. Acute rheumatic fever. Lancet. 2005. 366:155–168.
Article3. Logan D, McKee PJ. Poststreptococcal reactive arthritis. J am Podiatr Med Assoc. 2006. 96:362–366.
Article4. Moorthy LN, Gaur S, Peterson MG, Landa YF, Tandon M, Lehman TJ. Poststreptococcal reactive arthritis in children: a retrospective study. Clin Pediatr (Phila). 2009. 48:174–182.
Article5. Brahmadathan KN, Gladstone P. Microbiological diagnosis of streptococcal pharyngitis: lacunae and their implications. Indian J Med Microbiol. 2006. 24:92–96.
Article6. Jansen TL, Janssen M, de Jong AJ, Jeurissen ME. Post-streptococcal reactive arthritis: a clinical and serological description, revealing its distinction from acute rheumatic fever. J Intern Med. 1999. 245:261–267.
Article7. Robertson KA, Volmink JA, Mayosi BM. Antibiotics for the primary prevention of acute rheumatic fever: a meta-analysis. BMC Cardiovasc Disord. 2005. 5:11.
Article8. Steer AC, Carapetis JR. Prevention and treatment of rheumatic heart disease in the developing world. Nat Rev Cardiol. 2009. 6:689–698.
Article9. Inglis TJ. Decline in rheumatic fever. Lancet. 1985. 2:1005–1006.
Article10. Jose VJ, Gomathi M. Declining prevalence of rheumatic heart disease in rural schoolchildren in India: 2001-2002. Indian Heart J. 2003. 55:158–160.11. Olguntürk R, Aydin GB, Tunaoğlu FS, Akalin N. Rheumatic heart disease prevalence among schoolchildren in Ankara, Turkey. Turk J Pediatr. 1999. 41:201–206.12. Visser H, Speyer I, Ozcan B, Breedveld FC, van Ogtrop ML, Hazes JM. The diagnostic value of streptococcal serology in early arthritis: a prospective cohort study. Rheumatology. 2000. 39:1351–1356.
Article13. Waits JB. Rational use of laboratory testing in the initial evaluation of soft tissue and joint complaints. Prim Care. 2010. 37:673–689.
Article14. Omurzakova NA, Yamano Y, Saatova GM, Mirzakhanova MI, Shukurova SM, Kydyralieva RB, et al. High incidence of rheumatic fever and rheumatic heart disease in the republics of Central Asia. Int J Rheum Dis. 2009. 12:79–83.
Article15. Veasy LG, Wiedmeier SE, Orsmond GS, Ruttenberg HD, Boucek MM, Roth SJ, et al. Resurgence of acute rheumatic fever in the intermountain area of the United States. N Engl J Med. 1987. 316:421–427.
Article16. Danchin MH, Carlin JB, Devenish W, Nolan TM, Carapetis JR. New normal ranges of antistreptolysin O and antideoxyribonuclease B titres for Australian children. J Paediatr Child Health. 2005. 41:583–586.
Article17. Ayoub EM, Nelson B, Shulman ST, Barrett DJ, Campbell JD, Armstrong G, et al. Group A streptococcal antibodies in subjects with or without rheumatic fever in areas with high or low incidences of rheumatic fever. Clin Diagn Lab Immunol. 2003. 10:886–890.
Article18. Cha SH, Choi YM, Yang SW, Lee DH, Lee CG, Hong CH. Upper limit of normal value for antistreptolysin O titer of healthy children in Seoul. J Korean Pediatr Soc. 1995. 38:1061–1068.