Ann Rehabil Med.
2016 Apr;40(2):326-333. 10.5535/arm.2016.40.2.326.
Prevalence and Epidemiological Factors Involved in Cellulitis in Korean Patients With Lymphedema
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Kosin University College of Medicine, Busan, Korea. oggum@hanmail.net
- 2Department of Physical Medicine and Rehabilitation, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2309933
- DOI: http://doi.org/10.5535/arm.2016.40.2.326
Abstract
OBJECTIVE
To evaluate the prevalence and associated factors involved in cellulitis with lymphangitis among a group of Korean patients who were being treated for lymphedema. We present our epidemiologic research and we also report a systematic review of these types of cases.
METHODS
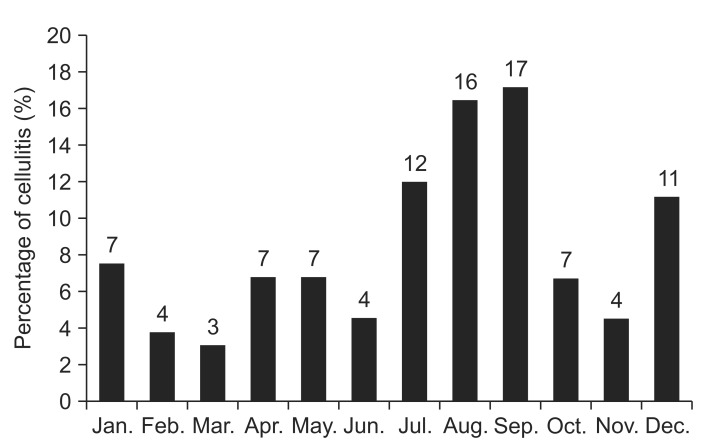
This was a retrospective medical record study among 1,246 patients diagnosed with lymphedema. The study was carried out between January 2006 and December 2012 at the Kosin University Gospel Hospital and Seoul National University Bundang Hospital. Cases were examined for onset time, affected site, seasonal trend, and recurrence pattern of lymphedema, lymphangitis, and cellulitis. We also evaluated the history of blood-cell culture and antibiotic use.
RESULTS
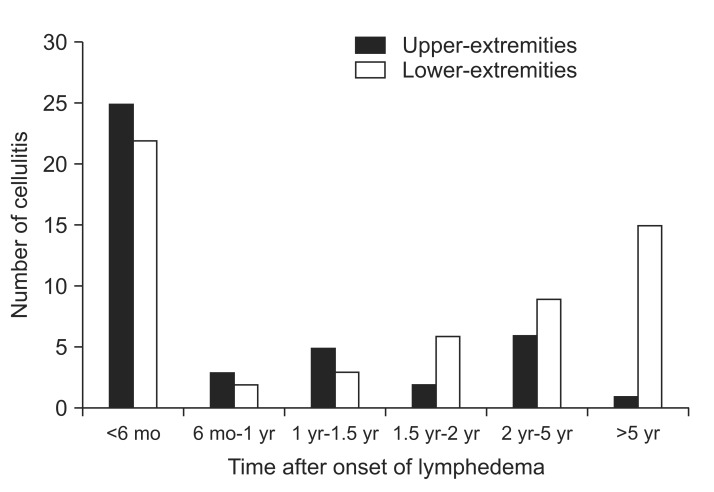
Ninety-nine lymphedema patients experienced complications such as cellulitis with accompanying lymphangitis. Forty-nine patients had more than two recurrences of cellulitis with lymphangitis. The incidence and recurrence of cellulitis with lymphangitis were significantly higher in the patients with lower-extremity lymphedema. There was a significant trend toward higher cellulitis prevalence in the lower-extremity lymphedema group according to the time of lymphedema onset. Among the cellulitis with lymphangitis cases, 62 cases were diagnosed through blood-cell culture; 8 of these 62 cultures were positive for β-hemolytic streptococci.
CONCLUSION
The prevalence rate of cellulitis with lymphangitis in patients with lymphedema was 7.95%, and the prevalence of recurrent episodes was 3.93%. Especially, there was high risk of cellulitis with lymphangitis after occurrence of lower-extremity lymphedema with passage of time. Lymphedema patients should be fully briefed about the associated risks of cellulitis before treatment, and physicians should be prepared to provide appropriate preventive education.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Reversible Splenial Lesion associated with Cellulitis in a Patient with Lymphedema
Ki-Hun Son, So-Young Lee, Won Gu Lee, Jin-Hyung Lee, Meyung-Kug Kim, Bong-Goo Yoo
J Neurocrit Care. 2017;10(2):136-139. doi: 10.18700/jnc.170023.
Reference
-
1. Smeltzer DM, Stickler GB, Schirger A. Primary lymphedema in children and adolescents: a follow-up study and review. Pediatrics. 1985; 76:206–218. PMID: 4022694.2. WHO Expert Committee on Filariasis. Lymphatic filariasis: fourth report of the WHO Expert Committee on Filariasis. World Health Organ Tech Rep Ser. 1984; 702:3–112. PMID: 6435317.3. Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008; 1131:147–154. PMID: 18519968.
Article4. Godoy JM, Silva SH, Godoy MF. Sensitivity and specificity of combined perimetric and volumetric evaluations in the diagnosis of arm lymphedema. Prague Med Rep. 2007; 108:243–247.5. Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004; 350:904–912. PMID: 14985488.6. Cox NH. Management of lower leg cellulitis. Clin Med (Lond). 2002; 2:23–27. PMID: 11871634.
Article7. Damstra RJ, van Steensel MA, Boomsma JH, Nelemans P, Veraart JC. Erysipelas as a sign of subclinical primary lymphoedema: a prospective quantitative scintigraphic study of 40 patients with unilateral erysipelas of the leg. Br J Dermatol. 2008; 158:1210–1215. PMID: 18363756.
Article8. Masmoudi A, Maaloul I, Turki H, Elloumi Y, Marrekchi S, Bouassida S, et al. Erysipelas after breast cancer treatment (26 cases). Dermatol Online J. 2005; 11:12. PMID: 16409908.
Article9. El Saghir NS, Otrock ZK, Bizri AR, Uwaydah MM, Oghlakian GO. Erysipelas of the upper extremity following locoregional therapy for breast cancer. Breast. 2005; 14:347–351. PMID: 15990307.
Article10. de Godoy JM, da Silva SH. Prevalence of cellulitis and erysipelas in post-mastectomy patients after breast cancer. Arch Med Sci. 2007; 3:249–251.11. de Godoy JM, de Godoy MF, Valente A, Camacho EL, Paiva EV. Lymphoscintigraphic evaluation in patients after erysipelas. Lymphology. 2000; 33:177–180. PMID: 11191659.12. Tsao H, Johnson RA. Bacterial cellulitis. Curr Opin Dermatol. 1997; 4:33–41.13. Dupuy A, Benchikhi H, Roujeau JC, Bernard P, Vaillant L, Chosidow O, et al. Risk factors for erysipelas of the leg (cellulitis): case-control study. BMJ. 1999; 318:1591–1594. PMID: 10364117.
Article14. Shih YC, Xu Y, Cormier JN, Giordano S, Ridner SH, Buchholz TA, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol. 2009; 27:2007–2014. PMID: 19289624.
Article15. Teerachaisakul M, Ekataksin W, Durongwatana S, Taneepanichskul S. Diet, C-reactive protein levels and cellulitis in patients with lymphedema: a cross-sectional study. J Med Med Sci. 2011; 2:1297–1301.16. Lewis SD, Peter GS, Gomez-Marin O, Bisno AL. Risk factors for recurrent lower extremity cellulitis in a U.S. Veterans Medical Center population. Am J Med Sci. 2006; 332:304–307. PMID: 17170620.
Article17. Scheinfeld NS. Obesity and dermatology. Clin Dermatol. 2004; 22:303–309. PMID: 15475230.
Article18. Bjornsdottir S, Gottfredsson M, Thorisdottir AS, Gunnarsson GB, Rikardsdottir H, Kristjansson M, et al. Risk factors for acute cellulitis of the lower limb: a prospective case-control study. Clin Infect Dis. 2005; 41:1416–1422. PMID: 16231251.
Article19. Duvanel T, Auckenthaler R, Rohner P, Harms M, Saurat JH. Quantitative cultures of biopsy specimens from cutaneous cellulitis. Arch Intern Med. 1989; 149:293–296. PMID: 2644902.
Article20. Moffatt CJ, Franks PJ, Doherty DC, Williams AF, Badger C, Jeffs E, et al. Lymphoedema: an underestimated health problem. QJM. 2003; 96:731–738. PMID: 14500859.
Article21. Soo JK, Bicanic TA, Heenan S, Mortimer PS. Lymphatic abnormalities demonstrated by lymphoscintigraphy after lower limb cellulitis. Br J Dermatol. 2008; 158:1350–1353. PMID: 18241266.
Article22. Collins PS, Villavicencio JL, Abreu SH, Gomez ER, Coffey JA, Connaway C, et al. Abnormalities of lymphatic drainage in lower extremities: a lymphoscintigraphic study. J Vasc Surg. 1989; 9:145–152. PMID: 2911134.
Article23. Woo PC, Lum PN, Wong SS, Cheng VC, Yuen KY. Cellulitis complicating lymphoedema. Eur J Clin Microbiol Infect Dis. 2000; 19:294–297. PMID: 10834819.
Article24. Badger C, Seers K, Preston N, Mortimer P. Antibiotics/anti-inflammatories for reducing acute inflammatory episodes in lymphoedema of the limbs. Cochrane Database Syst Rev. 2004; (2):CD003143. PMID: 15106193.
Article25. Baddour LM, Bisno AL. Non-group A beta-hemolytic streptococcal cellulitis: association with venous and lymphatic compromise. Am J Med. 1985; 79:155–159. PMID: 3875287.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reversible Splenial Lesion associated with Cellulitis in a Patient with Lymphedema
- The Effect of Stellate Ganglion Block on Breast Cancer-Related Infectious Lymphedema
- Typical Sweet Syndrome at the Site of Postmastectomy Lymphedema: Two Cases and a Literature Review
- Simple Congenital Lymphedema: A Case Report
- A Case of Lower Extremity Lymphedema in an Endstage Cancer Patient Complicated by Persistent Lymphorrhea