Korean J Urol.
2006 Jul;47(7):797-801. 10.4111/kju.2006.47.7.797.
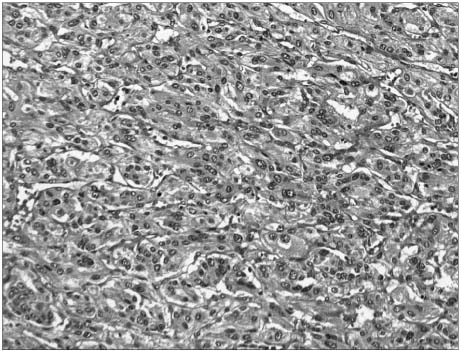
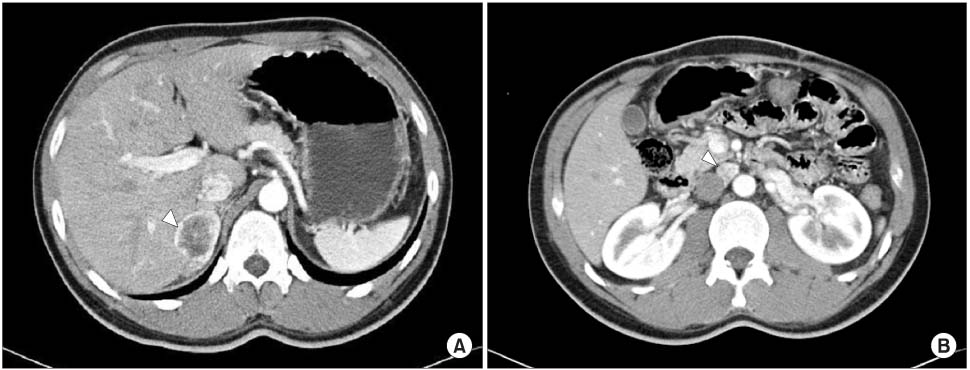
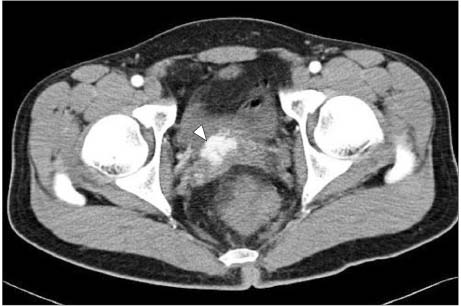
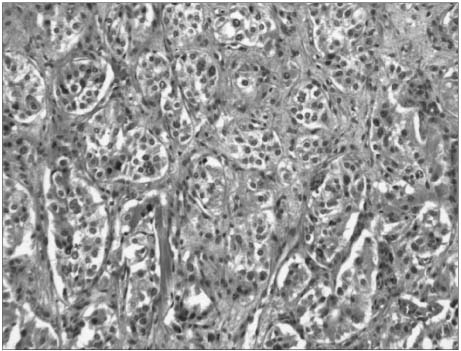
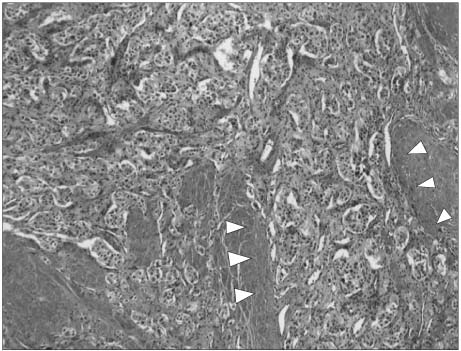
Malignant Pheochromocytoma that Recurred in the Contralateral Adrenal Gland and Metastasized to the Bladder
- Affiliations
-
- 1Department of Urology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. chung90@sanggyepaik.ac.kr
- 2Department of General Surgery, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of Diagnostic Radiology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 4Department of Pathology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2294326
- DOI: http://doi.org/10.4111/kju.2006.47.7.797
Abstract
- Pheochromocytoma is an uncommon neoplasm and it is derived from the neural crest. It is one of the surgically curable hypertensive syndromes. The sequela of this disease can be serious if definite treatment is not promptly performed. We report here on a case of malignant pheochromocytoma that recurred in the contralateral adrenal gland and it subsequently metastasized to the bladder after the patient refused treatment of the contralateral adrenal tumor.
Keyword
MeSH Terms
Figure
Reference
-
1. Goldstein RE, O'Neill JA Jr, Holcomb GW III, Morgan WM III, Neblett WW III, Oates JA, et al. Clinical experience over 48 years with pheochromocytoma. Ann Surg. 1999. 229:755–764.2. John H, Ziegler WH, Hauri D, Jaeger P. Pheochromocytomas: Can malignant potential be predicted? Urology. 1999. 53:679–683.3. Noshiro T, Shimizu K, Watanabe T, Akama H, Shibukawa S, Miura W, et al. Changes in clinical features and long-term prognosis in patients with pheochromocytoma. Am J Hypertens. 2000. 13:35–43.4. Lack EE. Lack EE, editor. Adrenal medullary hyperplasia and pheochromocytoma. Pathology of adrenal and extraadrenal paraganglia. Major problems in pathology. 1994. Philadelphia: WB Saunders;220–272.5. Thompson LD. Pheochromocytoma of the Adrenal Gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol. 2002. 26:551–566.6. Stenstrom G, Svardsudd K. Pheochromocytoma in Sweden 1958-1981. An analysis of the National Cancer Registry Data. Acta Med Scand. 1986. 220:220–232.7. Padmanabhan H, Ehrlich LD, Quazedo M, Fojo T, Louie A, Walther M, et al. Unusual locations of involvement by malignancies: case 2. Metastatic pheochromocytoma to the colon. J Clin Oncol. 2003. 21:3369–3371.8. Lee YS, Oh KH. Clinical evaluation of 12 cases of pheochromocytoma. Korean J Urol. 1993. 34:619–625.9. Mamede M, Carrasquillo JA, Chen CC, Corral PD, Whatley M, Ilias I, et al. Discordant localization of 2-[18F]-fluoro-2-deoxy-D-glucose in 6-[18F]-fluorodopamine- and [123I]-metaiodobenzylguanidine-negative metastatic pheochromocytoma sites. Nucl Med Commun. 2006. 27:31–36.10. Brouwers FM, Petricoin EF 3rd, Ksinantova L, Breza J, Rajapakse V, Ross S, et al. Low molecular weight proteomic information distinguishes metastatic from benign pheochromocytoma. Endocr Relat Cancer. 2005. 12:263–272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Malignant Pheochromocytoma
- A Case of Nonfunctioning Pheochromocytoma of the Bladder
- A Case of Adrenal Cystic Pheochromocytoma with Contralateral Adrenocortical Adenoma Causing Subclinical Cushing's Syndrome
- A Case of Pheochromocytoma
- Huge pheochromocytoma presented with paraaortic lymph node and spine metastases