Korean J Urol.
2006 Jul;47(7):740-746. 10.4111/kju.2006.47.7.740.
The Effect of Transurethral Resection of the Prostate in Detrusor Underactivity
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. LKS@smc.samsung.co.kr
- KMID: 2294315
- DOI: http://doi.org/10.4111/kju.2006.47.7.740
Abstract
-
PURPOSE: We evaluated the effect of transurethral resection of the prostate (TUR-P) in men with detrusor underactivity (DUA) who do not respond to conservative medical treatment.
MATERIALS AND METHODS
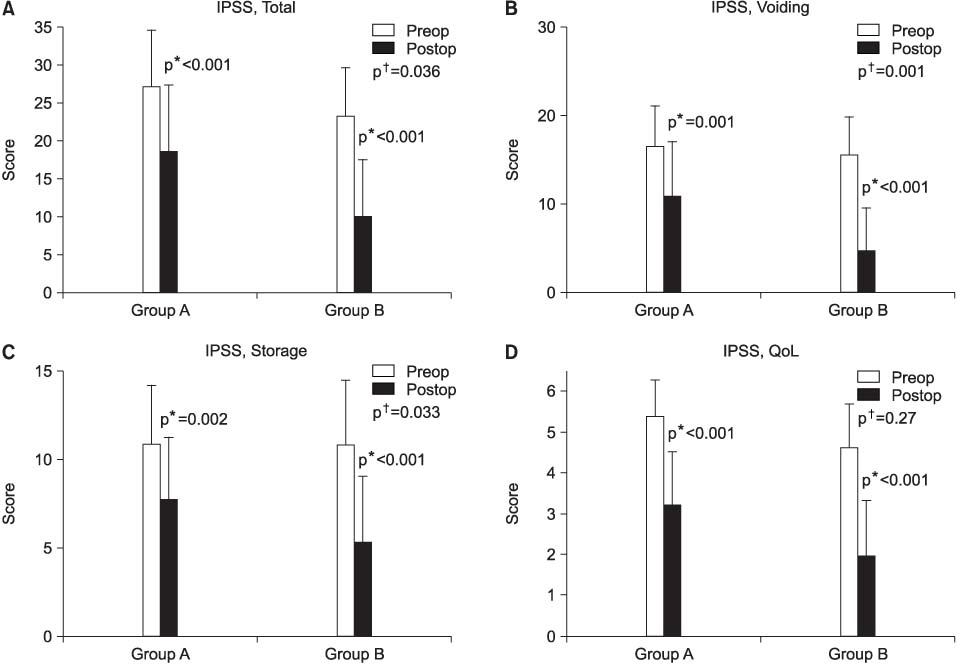
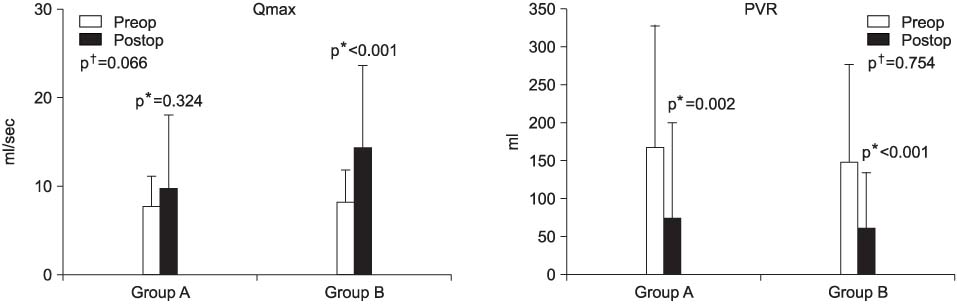
Of the patients who underwent TUR-P for LUTS at our institution, we reviewed the records of 71 patients who had undergone preoperative urodynamic study. According to the bladder outlet obstruction index and the bladder contractility index, the patients were divided into two groups: group A (25 patients) with unobstructed and underactive detrusor function, and group B (46 patients) with obstructed and/or normal detrusor contractility. We evaluated the difference of International Prostate Symptom Score (IPSS), quality of life (QoL), maximum flow rate (Qmax), post void residual (PVR) volume and the subjective satisfaction after TUR-P.
RESULTS
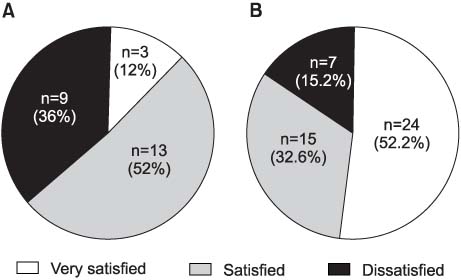
There were no significant differences preoperatively between the groups for age, Qmax and PVR. The total IPSS/QoL score was higher and the prostatic size was smaller in group A. After TUR-P in group A, the IPSS/QoL score and PVR were significantly improved; the Qmax was also improved, but this was not significant. There were significant improvements in all parameters in group B. Patients in group B showed the more significant improvement rate of the IPSS score and they were more satisfied after TUR-P than those in group A.
CONCLUSIONS
Patients with DUA had less improvement in their symptom score and operative satisfaction than those with obstructed and/or normal detrusor contractility after TUR-P. However, there was significant improvement in IPSS/QoL and PVR after TUR-P in former group and 64% of these patients were satisfied. Therefore, TUR-P is thought to be an optional surgical procedure for treating the men with DUA who do not respond to conservative medical treatment.
MeSH Terms
Figure
Cited by 1 articles
-
Epidemiology of underactive bladder: Common but underresearched
Young Dong Yu, Seong Jin Jeong
Investig Clin Urol. 2017;58(Suppl 2):S68-S74. doi: 10.4111/icu.2017.58.S2.S68.
Reference
-
1. Kanik EA, Erdem E, Abidinoglu D, Acar D, Akbay E, Ulusoy E. Can the outcome of transurethral resection of the prostate be predicted preoperatively? Urology. 2004. 64:302–305.2. Schäfer W, Noppeney R, Rübben H, Lutzeyer W. The value of free flow rate and pressure/flow-studies in the routine investigation of BPH patients. Neurourol Urodyn. 1988. 7:219–221.3. Rollema HJ, Van Mastrigt R. Improved indication and follow-up in transurethral resection of the prostate using the computer program CLIM: a prospective study. J Urol. 1992. 148:111–116.4. Griffiths D, Hofner K, van Mastrigt R, Rollema HJ, Spangberg A, Gleason D. Standardization of terminology of lower urinary tract function: pressure-flow studies of voiding, urethral resistance and urethral obstruction. Neurourol Urodyn. 1997. 16:1–18.5. Yamanish T, Yasuda K, Kamai T, Tsujii T, Sakakibara R, Uchiyama T, et al. Combination of a cholinergic drug and an alpha-blocker is more effective than monotherapy for the treatment of voiding difficulty in patients with underactive detrusor. Int J Urol. 2004. 11:88–96.6. Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int. 1999. 84:14–15.7. Ziada A, Rosenblum M, Crawford ED. Benign prostatic hyperplasia: an overview. Urology. 1999. 53:3 Suppl 3A. 1–6.8. Abrams P. In support of pressure-flow studies for evaluating men with lower urinary tract symptoms. Urology. 1994. 44:153–155.9. Lee JG, Shim KS, Koh SK. Incidence of detrusor underactivity in men with prostatism older than 50 years. Korean J Urol. 1999. 40:347–352.10. Lim CS, Abrams P. The Abrams-Griffiths nomogram. World J Urol. 1995. 13:34–39.11. Rodrigues P, Lucon AM, Freire GC. Urodynamic pressure flow studies can predict the clinical outcome after transurethral prostatic resection. J Urol. 2001. 165:499–502.12. Abrams PH. Prostatism and prostatectomy: the value of urine flow rate measurement in the preoperative assessment for operation. J Urol. 1977. 117:70–71.13. Abrams PH. The urodynamic changes following prostatectomy. Urol Int. 1978. 33:181–186.14. Javle P, Jenkins SA, Machin DG, Parsons KF. Grading of benign prostatic obstruction can predict the outcome of transurethral prostatectomy. J Urol. 1998. 160:1713–1717.15. Thomas AW, Cannon A, Bartlett E, Ellis-Jones J, Abrams P. The natural history of lower urinary tract dysfunction in men: the influence of detrusor underactivity on the outcome after transurethral resection of the prostate with a minimum 10-year urodynamic follow-up. BJU Int. 2004. 93:745–750.16. McConnell JD. Why pressure-flow studies should be optional and not mandatory studies for evaluating men with benign prostatic hyperplasia. Urology. 1994. 44:156–158.17. Bruskewitz RC, Jensen KM, Iversen P, Madsen PO. The relevance of minimum urethral resistance in prostatism. J Urol. 1983. 129:769–771.18. van Venrooij GE, van Melick HH, Eckhardt MD, Boon TA. Correlations of urodynamic changes in symptoms and well being after transurethral resection of the prostate. J Urol. 2002. 168:605–609.19. van Venrooij GE, van Melick HH, Boon TA. Comparison of outcomes of transurethral prostate resection in urodynamically obstructed versus selected urodynamically unobstructed or equivocal men. Urology. 2003. 62:672–676.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Surgical Outcomes Between Holmium Laser Enucleation and Transurethral Resection of the Prostate in Patients With Detrusor Underactivity
- The Urodynamic Findings of Male Patients with LUTS and the Effects of the Pre-operative Parameters on the Outcome of Transurethral Resection of the Prostate
- The Outcome and Satisfaction of Patients with Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia following Transurethral Resection of the Prostate according to Urodynamic Obstruction and the Bladder Function
- Potassium-Titanyl-Phosphate Laser Photoselective Vaporization of the Prostate in Patients with Benign Prostatic Hyperplasia with Detrusor Underactivity: Influence on Detrusor Pressure
- Clinical Observation on Transurethral Resection of Prostate and Suprapubic Prostatectomy for Benign Prostatic Hypertrophy