Korean J Urol.
2006 Feb;47(2):175-179. 10.4111/kju.2006.47.2.175.
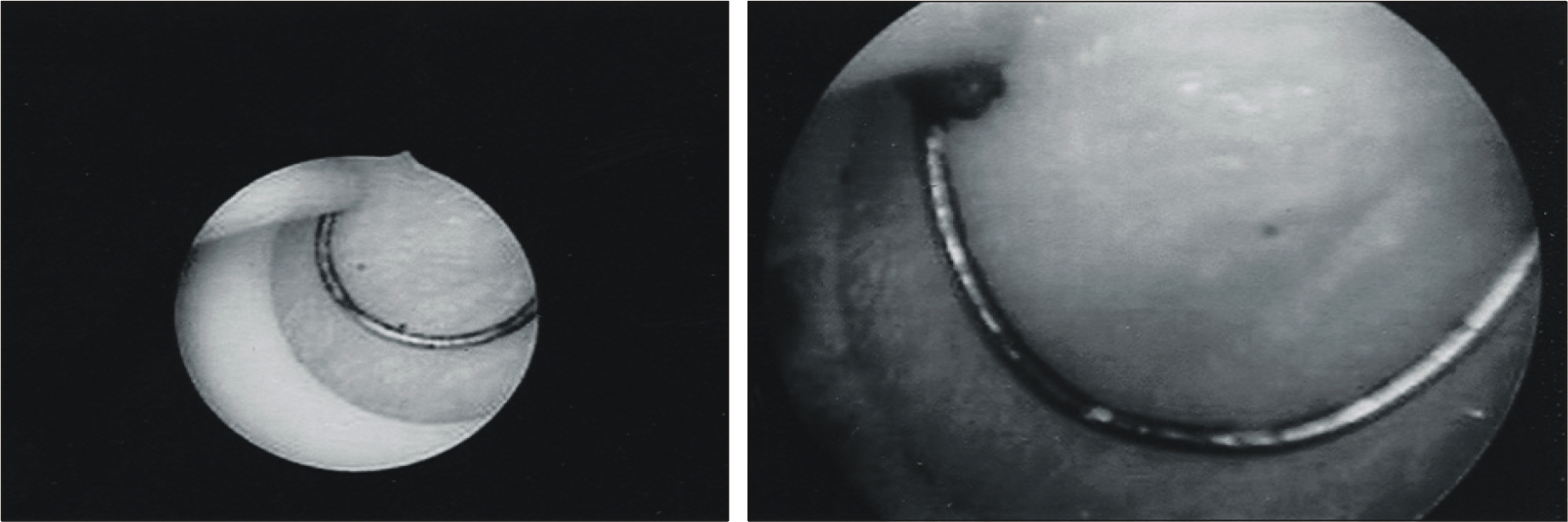
Transurethral Prostatectomy Using a 22F Continuous Running Irrigation System Resectoscope
- Affiliations
-
- 1Department of Urology, EulJi University School of Medicine, Eulji Medical Center, Seoul, Korea. ytk5202@eulji.or.kr
- KMID: 2294198
- DOI: http://doi.org/10.4111/kju.2006.47.2.175
Abstract
-
PURPOSE: The twenty-six F sized continuous running irrigation transurethral resection (TUR) system has showed a relatively high risk for inducing postoperative urethral stricture in Korean men. We evaluated the efficacy and safety of recently available 22F continuous running irrigation TUR system for treating benign prostatic hyperplasia (BPH) patients.
MATERIALS AND METHODS
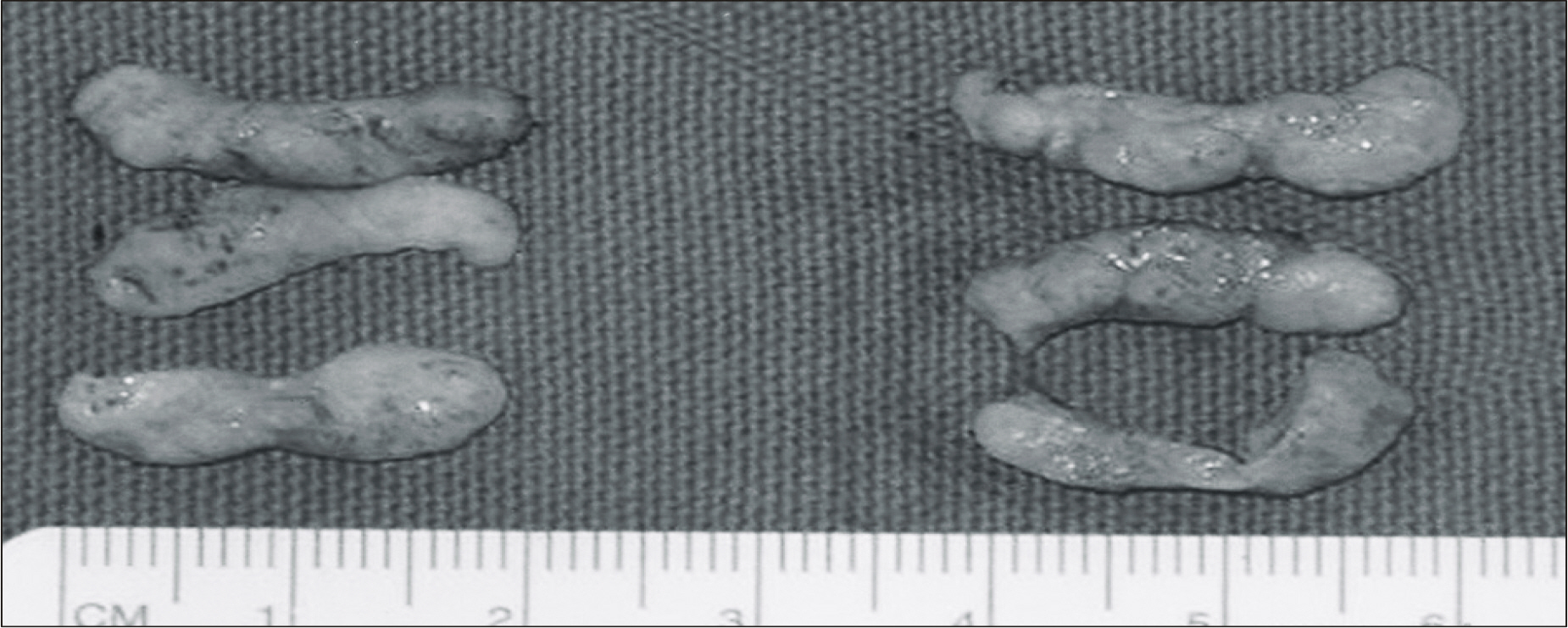
A total of seventy patients with severe symptomatic BPH underwent transurethral prostatectomy (TURP). The 26F system was used in 31 cases and the 22F system was used in 39 patients. The total resection weight, the resection rate, and the intraoperative and immediate postoperative complication rates were compared between the 2 groups. The patients were followed for 2 weeks, 4 weeks and 3 months postoperatively to check for the development of urethral stricture.
RESULTS
The total resection weight was 14.8+/-9.5gm in the 22F group and 11.2+/-10.2gm in the 26F group (p>0.05). The resection rates were 0.24+/-0.10gm/min and 0.19+/-0.11gm/min, respectively. The rate of urethral stricture requiring any type of management was 15.4% (6/39) in the 22F group and 38.7% (12/31) in the 26F group (p<0.05). Visual internal urethrotomy was performed in 2.6% (1/39) and 9.7% (3/31) of the patients, respectively. Other complications were 1 capsular perforation, 1 TUR syndrome, 1 epididymitis and 1 delayed bleeding in the 22F group, and 1 intraoperative fever and 1 epididymitis in the 26F group.
CONCLUSIONS
TURP using the 22F continuous running irrigation system enabled the surgeon to resect prostate adenoma with a similar speed and effectiveness as compared with the 26F system, and it significantly reduced the risk of urethral stricture. Performing TURP with using this system can be considered as a first line therapy for the BPH patients who require surgery.
MeSH Terms
Figure
Reference
-
1.Speakman MJ. Who should be treated and how? Evidence-based medicine in symptomatic BPH. Eur Urol. 1999. 36(Suppl 3):40–51.
Article2.Lee SB., Song KH., Song JM. Clinical assessment of transurethral resection of prostate (TURP) using continuous irrigation system. Korean J Urol. 2000. 41:1259–63.3.Lee DJ., Cho JS., Chung BS. An economic evaluation of pharmacological therapy and transurethral resection of the prostate for the treatment of benign prostatic hyperplasia. Korean J Urol. 2002. 43:619–23.4.Seo HK., Chung MK. Comparison of the effects of transurethral needle ablation and transurethral resection of the prostate for benign prostatic hyperplasia at 12 months follow-up. Korean J Urol. 2000. 41:414–9.5.Yang HT., Choi NG. Changes and differences of sexual function in patients with benign prostate hyperplasia following transurethral resection of prostate and high energy transurethral microwave thennotherapy. Korean J Urol. 2001. 42:961–6.6.Lee DK., Seong IG., Han BH. A clinical study about operator' s skilled experience in transurethral resection of benign prostatic hyperplasia. Korean J Urol. 1994. 35:626–31.7.Yoo TK. Transurethral prostatectomy by a novice resectionist. Korean J Urol. 1994. 35:991–7.8.Seoung IG., Han BH. Clinical results of transurethral resection for the benign prostatic hypertrophy-significance of suprapubic cystostomy before transurethral resection. Korean J Urol. 1987. 28:634–8.9.Sanchez Zalabardo JM., Sanchez Elipe MA., Regojo Zapata O., Elizalde Benito A., Valle Geriiold J., Lopez Lopez JA, et al. Modified technique for transurediral resection of the prostate with suprapubic drainage and local anesdiesia. Actas Urol Esp. 2003. 27:216–20.10.Yoo TK., Jung JY., Choi DY. A study for the urethral caliber in male adults visited urological outpatient department. Korean J Urol. 1999. 40(Suppl 2):220. abstract P-188.11.Chilton CP., Morgan RJ., England HR., Paris AM., Blandy JP. A critical evaluation of the results of transurethral resection of the prostate. Br J Urol. 1978. 50:542–6.
Article12.Mebust WK., Holtgrewe HL., Cocked: TK., Peters PC. Transurethral prostatectomy: immediate and postoperative complications: a cooperative study of 13 participating institutions evaluating 3, 885 patients. J Urol. 1989. 141:243–7.13.Nielsen KK., Nordling J. Urethral stricture following transurethral prostatectomy. Urology. 1990. 35:18–24.14.Walton JK., Wright WL., Robinson RG., Nacey JN. The meatal problem with TUR prostate: the value of postoperative selfdilatation. Br J Urol. 1984. 56:202–7.15.Desmond AD., Evans CM., Jameson RM., Woolfenden KA., Gibbon NO. Critical evaluation of direct vision uredirotomy by urine flow measurement. Br J Urol. 1981. 53:630–3.16.Jorgensen PE., Weis N., Bruun E. Etiology of urethral stricture following transurethral prostatectomy. A retrospective study. Scand J Urol Nephrol. 1986. 20:253–5.17.Hammarsten J., Lindqvist K., Sunzel H. Urethral strictures following transurediral resection of the prostate. The role of the catheter. Br J Urol. 1989. 63:397–400.18.Balbay MD., Ergen A., Sahin A., Lekili M., Ulucay S., Kara-agaoglu E. Development of urethral stricture after transurediral prostatectomy: a retrospective study. Int Urol Nephrol. 1992. 24:49–53.19.Schultz A., Bay-Nielsen H., Bilde T., Christiansen L., Mikkelsen AM., Steven K. Prevention of urethral stricture formation after transurediral resection of the prostate: a controlled randomized study of Otis urethrotomy versus urethral dilation and the use of the polytetrafluoroediylene coated versus the uninsulated metal sheath. J Urol. 1989. 141:73–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation on Transurethral Resection of Prostate and Suprapubic Prostatectomy for Benign Prostatic Hypertrophy
- Clinical Observation and Comparison Between the Results of Transurethral Resection and Open Prostatectomy on the Benign Prostatic Hypertrophy
- The assessment of symptomatic improvement of patients with benign prostatic hyperplasia after transurethral prostatectomy
- The Experimental Studies for the Effects of the Continuous Irrifation Method to Normal Tissue
- Predictive Factors Affecting Urethral Stricture Development after Transurethral Resection of the Prostate in Patients with Benign Prostatic Hyperplasia