Korean J Urogenit Tract Infect Inflamm.
2013 Apr;8(1):13-19. 10.14777/kjutii.2013.8.1.13.
Asymptomatic Prostatitis: Clinical Significances and Management
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea. drmsk@korea.com
- KMID: 2289247
- DOI: http://doi.org/10.14777/kjutii.2013.8.1.13
Abstract
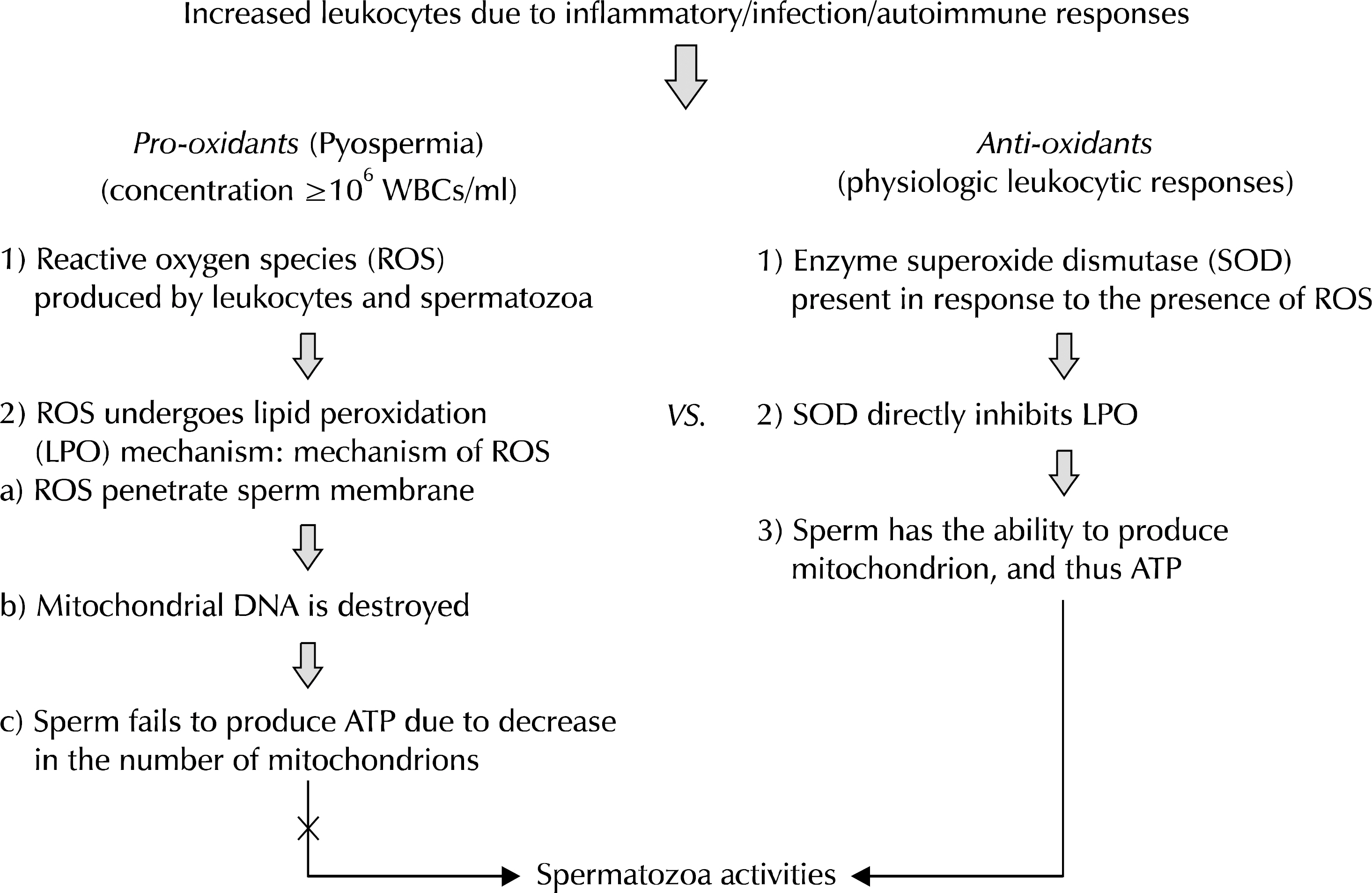
- Asymptomatic inflammatory prostatitis (National Institutes of Health, category IV) has been introduced as a separate clinical entity among other prostatitis syndromes. Asymptomatic inflammatory prostatitis is characterized by the presence of significant amount of leukocytes (white blood cells) in prostate-specific samples (post-prostatic massage urine, expressed prostatic secretion, semen, and prostate biopsy) but no subjective symptoms are found, and is therefore diagnosed solely in the laboratory. There have been many questions regarding the clinical role of asymptomatic inflammatory prostatitis and its impact on the management of prostate disease and sterility. This review presents the current definition of asymptomatic inflammatory prostatitis, summarizes the clinical evidence on the two important issues prostate specific antigen and pyospermia, and discusses the optimal approaches to reduce its confounding impact on prostate cancer screening and indiscriminate use of antibiotics.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prevalence of
Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, Ureaplasma urealyticum in Chronic Prostatitis Category IIIa and IIIb Patients Using Polymerase Chain Reaction
In-Chang Cho, Yoo Seok Kim, Sung Bin Kim, Soon Ki Kim, Gyeong In Lee, Seung Ki Min
Korean J Urogenit Tract Infect Inflamm. 2013;8(2):102-108. doi: 10.14777/kjutii.2013.8.2.102.
Reference
-
1. Krieger JN, Riley DE, Cheah PY, Liong ML, Yuen KH. Epidemiology of prostatitis: new evidence for a world-wide problem. World J Urol. 2003; 21:70–4.2. Woo YN. Prostatitis. Korean J Urol. 1994; 35:575–85.3. Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001; 165:842–5.
Article4. Nadler RB, Schaeffer AJ. Lower urinary tract cultures. Nickel JC, editor. Textbook of Prostatitis. Oxford, England: Isis Medical Media;1999. p. 201–6.5. Polascik TJ, Oesterling JE, Partin AW. Prostate specific antigen: a decade of discovery–what we have learned and where we are going. J Urol. 1999; 162:293–306.
Article6. Kawakami J, Siemens DR, Nickel JC. Prostatitis and prostate cancer: implications for prostate cancer screening. Urology. 2004; 64:1075–80.
Article7. Kandirali E, Boran C, Serin E, Semercioz A, Metin A. Association of extent and aggressiveness of inflammation with serum PSA levels and PSA density in asymptomatic patients. Urology. 2007; 70:743–7.
Article8. Aitken RJ. A free radical theory of male infertility. Reprod Fertil Dev. 1994; 6:19–23.
Article9. Barratt CL, Bolton AE, Cooke ID. Functional significance of white blood cells in the male and female reproductive tract. Hum Reprod. 1990; 5:639–48.
Article10. Wolff H, Anderson DJ. Immunohistologic characterization and quantitation of leukocyte subpopulations in human semen. Fertil Steril. 1988; 49:497–504.11. Shy KK, Stenchever MA, Muller CH. Sperm penetration assay and subsequent pregnancy: a prospective study of 74 infertile men. Obstet Gynecol. 1988; 71:685–90.12. Sigman M, Lopes L. The correlation between round cells and white blood cells in the semen. J Urol. 1993; 149:1338–40.
Article13. Budía A, Luis Palmero J, Broseta E, Tejadillos S, Benedicto A, Queipo JA, et al. Value of semen culture in the diagnosis of chronic bacterial prostatitis: a simplified method. Scand J Urol Nephrol. 2006; 40:326–31.
Article14. Okada K, Matsumoto K. Effect of dietary salt restriction on tubular hypertrophy in rats with early-stage chronic renal failure. Scand J Urol Nephrol. 2004; 38:326–31.
Article15. Brawn PN, Speights VO, Kuhl D, Riggs M, Spiekerman AM, McCord RG, et al. Prostate-specific antigen levels from completely sectioned, clinically benign, whole prostates. Cancer. 1991; 68:1592–9.
Article16. Irani J, Levillain P, Goujon JM, Bon D, Dore B, Aubert J. Inflammation in benign prostatic hyperplasia: correlation with prostate specific antigen value. J Urol. 1997; 157:1301–3.
Article17. Kwak C, Ku JH, Kim T, Park DW, Choi KY, Lee E, et al. Effect of subclinical prostatic inflammation on serum PSA levels in men with clinically undetectable prostate cancer. Urology. 2003; 62:854–9.
Article18. Nickel JC, Shoskes D, Wang Y, Alexander RB, Fowler JE Jr, Zeitlin S, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006; 176:119–24.
Article19. Schatteman PH, Hoekx L, Wyndaele JJ, Jeuris W, Van Marck E. Inflammation in prostate biopsies of men without prostatic malignancy or clinical prostatitis: correlation with total serum PSA and PSA density. Eur Urol. 2000; 37:404–12.20. Simardi LH, Tobias-MacHado M, Kappaz GT, Taschner Goldenstein P, Potts JM, Wroclawski ER. Influence of asymptomatic histologic prostatitis on serum prostate-specific antigen: a prospective study. Urology. 2004; 64:1098–101.
Article21. Yaman O, Gogus C, Tulunay O, Tokatli Z, Ozden E. Increased prostate-specific antigen in subclinical prostatitis: the role of aggressiveness and extension of inflammation. Urol Int. 2003; 71:160–4.
Article22. Schaeffer AJ, Wu SC, Tennenberg AM, Kahn JB. Treatment of chronic bacterial prostatitis with levofloxacin and ciprofloxacin lowers serum prostate specific antigen. J Urol. 2005; 174:161–4.
Article23. Serretta V, Catanese A, Daricello G, Liotta R, Allegro R, Martorana A, et al. PSA reduction (after antibiotics) permits to avoid or postpone prostate biopsy in selected patients. Prostate Cancer Prostatic Dis. 2008; 11:148–52.
Article24. World Health Organization. WHO semen manual for the examination of human semen and cervical mucus. Cambridge: Cambridge University Press. 1992. 8–11.25. Berger RE, Karp LE, Williamson RA, Koehler J, Moore DE, Holmes KK. The relationship of pyospermia and seminal fluid bacteriology to sperm function as reflected in the sperm penetration assay. Fertil Steril. 1982; 37:557–64.26. Maruyama DK Jr, Hale RW, Rogers BJ. Effects of white blood cells on the in vitro penetration of zona-free hamster eggs by human spermatozoa. J Androl. 1985; 6:127–35.27. Wolff H, Politch JA, Martinez A, Haimovici F, Hill JA, Anderson DJ. Leukocytospermia is associated with poor semen quality. Fertil Steril. 1990; 53:528–36.
Article28. Pentyala S, Lee J, Annam S, Alvarez J, Veerraju A, Yadlapalli N, et al. Current perspectives on pyospermia: a review. Asian J Androl. 2007; 9:593–600.
Article29. Villegas J, Schulz M, Soto L, Iglesias T, Miska W, Sanchez R. Influence of reactive oxygen species produced by activated leukocytes at the level of apoptosis in mature human spermatozoa. Fertil Steril. 2005; 83:808–10.
Article30. Kopa Z, Wenzel J, Papp GK, Haidl G. Role of granulocyte elastase and interleukin-6 in the diagnosis of male genital tract inflammation. Andrologia. 2005; 37:188–94.
Article31. Micic S, Macura M, Lalic N, Dotlic R. Elastase as an indicator of silent genital tract infection in infertile men. Int J Androl. 1989; 12:423–9.
Article32. Arata de Bellabarba G, Tortolero I, Villarroel V, Molina CZ, Bellabarba C, Velazquez E, et al. Nonsperm cells in human semen and their relationship with semen parameters. Arch Androl. 2000; 45:131–6.33. Fisch H, Lipshultz LI. Diagnosing male factors of infertility. Arch Pathol Lab Med. 1992; 116:398–405.34. Henkel R, Maass G, Hajimohammad M, Menkveld R, Stalf T, Villegas J, et al. Urogenital inflammation: changes of leucocytes and ROS. Andrologia. 2003; 35:309–13.
Article35. Brunet J, Farine JC, Garay RP, Hannaert P. In vitro antioxidant properties of calcium dobesilate. Fundam Clin Pharmacol. 1998; 12:205–12.
Article36. Iinuma S, Naito Y, Yoshikawa T, Takahashi S, Takemura T, Yoshida N, et al. In vitro studies indicating antioxidative properties of rebamipide. Dig Dis Sci. 1998; 43(9 Suppl):35S–39S.37. Zheng RL, Zhang H. Effects of ferulic acid on fertile and asthenozoospermic infertile human sperm motility, viability, lipid peroxidation, and cyclic nucleotides. Free Radic Biol Med. 1997; 22:581–6.
Article38. Yamamoto M, Hibi H, Katsuno S, Miyake K. Antibiotic and ejaculation treatments improve resolution rate of leukocytospermia in infertile men with prostatitis. Nagoya J Med Sci. 1995; 58:41–5.39. Yanushpolsky EH, Politch JA, Hill JA, Anderson DJ. Antibiotic therapy and leukocytospermia: a prospective, randomized, controlled study. Fertil Steril. 1995; 63:142–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Guideline for the Diagnosis and Treatment of Urinary Tract Infections: Asymptomatic Bacteriuria, Uncomplicated & Complicated Urinary Tract Infections, Bacterial Prostatitis
- Prostatitis
- Chronic Prostatitis: A Possible Cause of Hematospermia
- The Concentrations of Zinc in Expressed Prostatic Secretion of Chronic Prostatitis Patients
- Clinical Effects of Serenoa Repens(Permixon) on Chronic Prostatitis