J Breast Cancer.
2006 Dec;9(4):349-353. 10.4048/jbc.2006.9.4.349.
The analgesic effects of intercostal nerve block in patients undergoing augmentation mammoplasty: MDbP 203
- KMID: 2286608
- DOI: http://doi.org/10.4048/jbc.2006.9.4.349
Abstract
-
PURPOSE: Augmentation mammoplasty is a procedure that expands the breast tissue and pectoral muscle by insertion of an implant. This procedure induce extreme postoperative pain. The purpose of this study was to determine whether intercostal nerve block (ICNB) could reduce the pain after augmentation mammoplasty.
METHODS
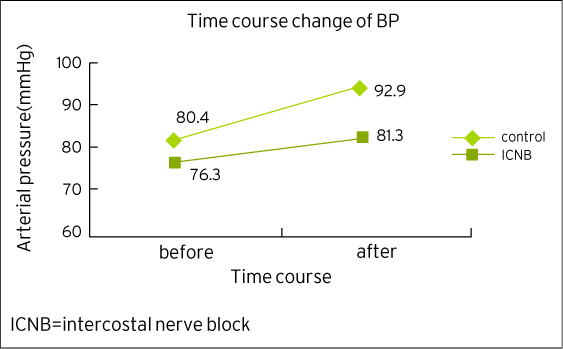
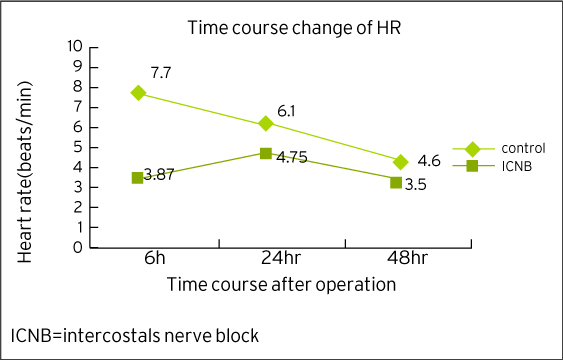
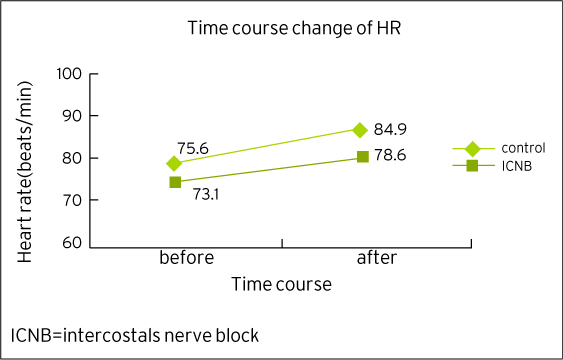
Eighty three patients, who underwent augmentation mammoplasty, at the M.D. Clinic between December 2005 and February 2006, were the cases of this study. We injected 0.25% ropivacaine (total 30ml per side) in the ICNB group (n=68) into the 3,4,5 and 6th intercostals spaces following induction of general anesthesia for surgery. The mean arterial pressures and heart rates were measured before and after subpectoral dissection. A numerical rating scale (NRS: 0=no pain, 10= most severe pain) was used to measure the pain postoperative 6, 24, 48 hours, respectively. We statistically compared the ICNB group with the control group (n=15) with using the Mann-Whitney Rank Sum test.
RESULTS
The mean arterial pressures and heart rates were more stable during subpectoral dissection in the ICNB group than in the control group (p= 0.142 and p= 0.037). The NRSs were lower throughout the 48 hours of the postoperative period in the ICNB group than in the control group (p<0.001 at 6hr, p=0.017 at 24hr, p=0.054 at 48hr).
CONCLUSION
ICNB induced stable vital sign during subpectoral dissection and excellent postoperative pain control during 48 hours postoperatively for those patients undergoing augmentation mammoplasty.
MeSH Terms
Figure
Reference
-
1. Perttunen K, Nilsson E, Heinonen J, Hirvisalo EL, Salo JA, Kalso E. Extradural, paravertebral and intercostals nerve blocks for post-thoracotomy pain. Br J Anaesth. 1995. 75:541–547.
Article2. Tschernko EM, Klepetko H, Grunder E, Kritzinger M, Klimscha W, Jandrasits O, et al. Clonidine added to the anesthetic solution enhances analgesia improves oxygenation after intercostals nerve block for thoracotomy. Anesth Analg. 1998. 87:107–111.
Article3. Pacik PT, Werner C. Pain control in augmentation mammaplasty: the use of indwelling catheters in 350 consecutive patients. Plast Reconstr Surg. 2005. 115:575–577.
Article4. Pacik PT, Werner C, Jackson N, Lobsitz C. Pain control in augmentation mammaplasty: The use of indwelling catheters in 200 consecutive patients. Plast Reconstr Surg. 2003. 111:2090–2096.
Article5. Papanastasiou S, Evans J. Postoperative analgesia in augmentation mammaplasty. Plast Reconstr Surg. 2000. 105:1241.
Article6. Schneider MS. Pain reduction in breast augmentation using methocarbamol. Aesthetic Plast Surg. 1997. 21:23–24.
Article7. Huang TT, Parks DH, Lewis SR. Outpatient breast surgery under intercostals block anesthesia. Plast Reconstr Surg. 1979. 62:299–303.8. Atanassoff PG, Alon E, Pasch T, Ziegler WH, Gautschi K. Intercostal nerve block for minor breast surgery. Reg Anesth. 1991. 16:23–27.9. Kolawole IK, Adesina MD, Olaoye IO. Intercostal nerve block for mastectomy in two patients with advanced breast malignancy. J Natl Med Assoc. 2006. 98:450–453.10. Craig DB. Postoperative recovery of pulmonary function. Anesth Analg. 1981. 60:46–52.11. Conacher ID. Pain relief after thoracotomy. Br J Anaesth. 1990. 65:806–812.
Article12. Shim KD, Kwon SY, Lee JS, Lee JI, Chang DJ, Lee YW. The analgesic effects of intercostals nerve block in patients undergoing total ear reconstruction. Korean J Anesth. 2003. 46:170–174.
Article13. McClure JH. Ropivacaine. Br J Anaesth. 1996. 76:300–307.
Article14. Whiteside JB, Wildsmith JA. Developments in local anaesthetic drugs. Br J Anaesth. 2001. 87:27–35.
Article15. Budzynski TH, Stoyva JM, Adler CS, Mullaney DJ. EMG biofeedback and tension headache: a controlled outcome study. Psycosom Med. 1973. 35:484–496.
Article16. Melzack R. The McGill pain questionnaire: major properties and scoring methods. Pain. 1975. 1:277–299.
Article17. Bernards CM. Barash PG, Cullen BF, Stoelting RK, editors. Epidural and spinal anesthesia. Clinical Anesthesia. 2001. 4th ed.Philadelphia: Lippincott Williams & Wilkins;702.18. Dahl JB, Kehlet H. The value of pre-emptive analgesia in the treatment of postoperative pain. Br J Anaesth. 1993. 70:434–439.
Article19. Doyle E, Bowler GM. Pre-emptive effect of multimodal analgesia in thoracic surgery. Br J Anaesth. 1998. 80:147–151.
Article20. Woolf CJ, Chong MS. Preemptive analgesia-treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993. 77:362–379.
Article21. Moore DC. Pneumothorax. Its incidence following intercostals nerve block. JAMA. 1962. 182:1005–1008.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report
- The Analgesic Effects of Intercostal Nerve Block in Patients Undergoing Total Ear Reconstruction
- Effects of Intercostal Nerve Block Combined with IV-PCA on Pain and Inspiratory Capacity after Thoracotomy
- Endoscopically Assisted Transumbilical Subpectoral Augmentation Mammoplasty
- Intercostal nerve transfer for the treatment of brachial plexus injury