J Breast Cancer.
2010 Dec;13(4):357-365. 10.4048/jbc.2010.13.4.357.
The Clinical Use of Low-Dose Multidetector Row Computed Tomography for Breast Cancer Patients in the Prone Position
- Affiliations
-
- 1Department of Radiology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea. seoboky@korea.ac.kr
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 5Department of General Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- KMID: 2286523
- DOI: http://doi.org/10.4048/jbc.2010.13.4.357
Abstract
- PURPOSE
To investigate the clinical use of low-dose multidetector row computed tomography (MDCT) for staging of invasive breast cancers with patients in the prone position.
METHODS
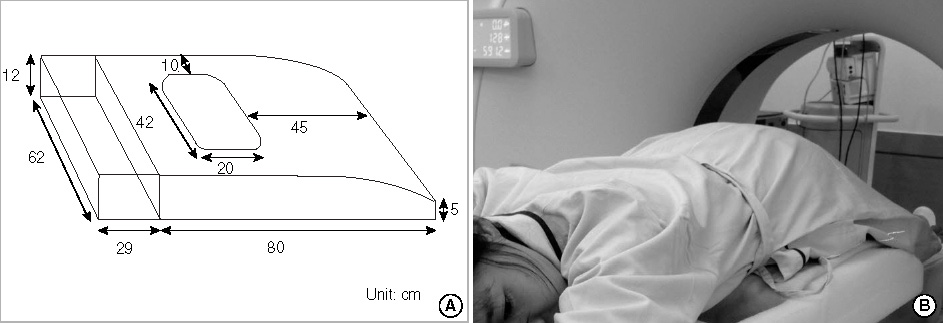
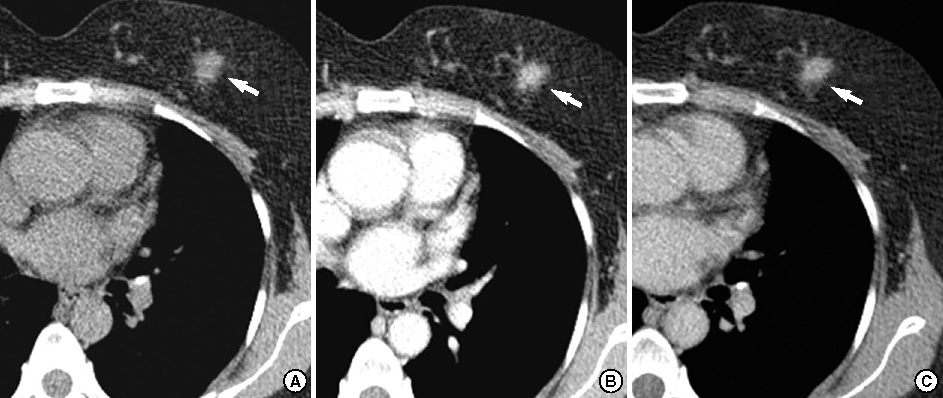
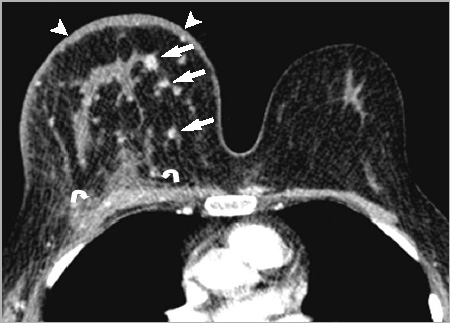
Three hundred twenty-two patients with 334 pathologically-verified breast cancers had low-dose MDCT breast imaging in the prone position for tumor staging before treatment between May 2006 and June 2010. We designed an additional computed tomography table pad with a hole for prone positioning. Patients lay prone on the table pad and the breasts were positioned within the rectangular hole. We obtained dynamic breast imaging from the lower neck to the lung base with the following parameters: 120 kVp, 50 mAs, and 3-mm reconstruction intervals. We evaluated the extent of the primary tumor, lymph nodal status, and distant metastasis in lung or bone, then assessed tumor staging based on the TNM classification of breast cancer. The assessed staging compared to the pathologic results for diagnostic accuracy.
RESULTS
Among the 334 invasive breast cancers, the overall diagnostic accuracy of tumor staging was 88.3% and the accuracy values of each tumor stage were 89.6% in T1, 90.8% in T2, 81.0% in T3, and 89.3% in T4. The overall diagnostic accuracy of lymph nodal staging was 86.3% and the accuracy values in each nodal stage were 82.9% in N0, 88.0% in N1, 89.7% in N2, and 93.3% in N3. Based on breast computed tomography scans, we detected distant metastases in 30 cases (7 lungs, 10 bones, 7 lungs and bones, and 6 livers).
CONCLUSION
Low-dose MDCT scanning for invasive breast cancer patients in the prone position is a feasible imaging technique for tumor staging before treatment to evaluate primary breast tumors, lymph nodes, lungs, or thoracic bones with reduced radiation doses.
MeSH Terms
Figure
Cited by 1 articles
-
Lymphoma Affecting the Breast: A Pictorial Review of Multimodal Imaging Findings
Euddeum Shim, Sung Eun Song, Bo Kyoung Seo, Young-Sik Kim, Gil Soo Son
J Breast Cancer. 2013;16(3):254-265. doi: 10.4048/jbc.2013.16.3.254.
Reference
-
1. Akashi-Tanaka S, Fukutomi T, Miyakawa K, Uchiyama N, Tsuda H. Diagnostic value of contrast-enhanced computed tomography for diagnosing the intraductal component of breast cancer. Breast Cancer Res Treat. 1998. 49:79–86.
Article2. Uematsu T, Sano M, Homma K, Makino H, Shiina M, Kobayashi S, et al. Staging of palpable T1-2 invasive breast cancer with helical CT. Breast Cancer. 2001. 8:125–130.
Article3. Inoue T, Tamaki Y, Hamada S, Yamamoto S, Sato Y, Tamura S, et al. Usefulness of three-deminsional multidetector-row CT images for preoperative evaluation of tumor extension in primary breast cancer patients. Breast Cancer Res Treat. 2005. 89:119–125.
Article4. Hagay C, Cherel PJ, de Maulmont CE, Plantet MM, Gilles R, Floiras JL, et al. Contrast-enhanced CT: value for diagnosing local breast cancer recurrence after conservative treatment. Radiology. 1996. 200:631–638.
Article5. Cheng JC, Cheng SH, Lin KJ, Jian JJ, Chan KY, Huang AT. Diagnostic thoracic-computed tomography in radiotherapy for loco-regional recurrent breast carcinoma. Int J Radiat Oncol Biol Phys. 1998. 41:607–613.
Article6. Kang DK, Kim MJ, Jung YS, Yim H. Clinical application of multidetector row computed tomography in patients with breast cancer. J Comput Assist Tomogr. 2008. 32:583–598.
Article7. Seo BK, Pisano ED, Cho KR, Cho PK, Lee JY, Kim SJ. Low-dose multidetector dynamic CT in the breast preliminary study. Clin Imaging. 2005. 29:172–178.8. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 2010. 7th ed. New York: Springer-Verlag.9. NCCN guidelines for treatment of cancer by site. National Comprehensive Cancer Network. accessed Nov 10, 2010. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.10. Obdeijn IM, Kuijpers TJ, van Dijk P, Wiggers T, Oudkerk M. MR lesion detection in a breast cancer population. J Magn Reson Imaging. 1996. 6:849–854.
Article11. Boné B, Péntek Z, Perbeck L, Veress B. Diagnostic accuracy of mammography and contrast-enhanced MR imaging in 238 histologically verified breast lesions. Acta Radiol. 1997. 38:489–496.
Article12. Heywang-Köbrunner SH, Viehweg P, Heinig A, Kuchler C. Contrastenhanced MRI of the breast: accuracy, value, controversies, solutions. Eur J Radiol. 1997. 24:94–108.
Article13. Lindfors KK, Boone JM, Nelson TR, Yang K, Kwan AL, Miller DF. Dedicated breast CT: initial clinical experience. Radiology. 2008. 246:725–733.
Article14. Boone JM, Nelson TR, Lindfors KK, Seibert JA. Dedicated breast CT: radiation dose and image quality evaluation. Radiology. 2001. 221:657–667.
Article15. Inoue M, Sano T, Watai R, Ashikaga R, Ueda K, Watatani M, et al. Dynamic multidetector CT of breast tumors: diagnostic features and comparison with conventional techniques. AJR Am J Roentgenol. 2003. 181:679–686.
Article16. Kuhl C, Kuhn W, Braun M, Schild H. Pre-operative staging of breast cancer with breast MRI: one step forward, two steps back? Breast. 2007. 16:Suppl 2. S34–S44.
Article17. Lim HI, Choi JH, Yang JH, Han BK, Lee JE, Lee SK, et al. Does preoperative breast magnetic resonance imaging in addition to mammography and breast ultrasonography change the operative management of breast carcinoma? Breast Cancer Res Treat. 2010. 119:163–167.
Article18. Uematsu T, Sano M, Homma K, Shiina M, Kobayashi S. Three-dimensional helical CT of the breast: accuracy for measuring extent of breast cancer candidates for breast conserving surgery. Breast Cancer Res Treat. 2001. 65:249–257.
Article19. Nakahara H, Namba K, Wakamatsu H, Watanabe R, Furusawa H, Shirouzu M, et al. Extension of breast cancer: comparison of CT and MRI. Radiat Med. 2002. 20:17–23.20. Taira N, Ohsumi S, Takabatake D, Hara F, Takashima S, Aogi K, et al. Contrast-enhanced CT evaluation of clinically and mammographically occult multiple breast tumors in women with unilateral early breast cancer. Jpn J Clin Oncol. 2008. 38:419–425.
Article21. Mortellaro VE, Marshall J, Singer L, Hochwald SN, Chang M, Copeland EM, et al. Magnetic resonance imaging for axillary staging in patients with breast cancer. J Magn Reson Imaging. 2009. 30:309–312.
Article22. Alvarez S, Añorbe E, Alcorta P, López F, Alonso I, Cortés J. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol. 2006. 186:1342–1348.
Article23. American College of Radiology. ACR Practice Guideline for the Performance of Screening Mammography. 2006. Reston: American College of Radiology;217–225.24. Hurwitz LM, Yoshizumi TT, Goodman PC, Nelson RC, Toncheva G, Nguyen GB, et al. Radiation dose savings for adult pulmonary embolus 64-MDCT using bismuth breast shields, lower peak kilovoltage, and automatic tube current modulation. AJR Am J Roentgenol. 2009. 192:244–253.
Article25. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991. 21:1–201.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Dosimetric Parameters of Patient with Large and Pendulous Breast Receiving Breast Radiotherapy in the Prone versus Supine Position
- Korean First Prospective Phase II Study, Feasibility of Prone Position in Postoperative Whole Breast Radiotherapy: A Dosimetric Comparison
- The Supine and Prone Position for Computed Tomographic Myelography(CTM) of the Lumbar Spine: Change of Gantry Angle
- Sacroiliitis in Ankylosing Spondylitis: Comparison with Multidetector Row CT and Plain Radiography
- Multidetector Row CT Findings of a Sternal Variation