J Breast Cancer.
2012 Mar;15(1):119-123. 10.4048/jbc.2012.15.1.119.
Medical and Surgical Treatment of Idiopathic Granulomatous Lobular Mastitis: A Benign Inflammatory Disease Mimicking Invasive Carcinoma
- Affiliations
-
- 1Department of Surgery, Haydarpasa Numune Teaching and Research Hospital, Istanbul, Turkey. ggurleyik@yahoo.com
- 2Department of Pathology, Haydarpasa Numune Teaching and Research Hospital, Istanbul, Turkey.
- 3Department of Radiology, Haydarpasa Numune Teaching and Research Hospital, Istanbul, Turkey.
- KMID: 2286483
- DOI: http://doi.org/10.4048/jbc.2012.15.1.119
Abstract
- PURPOSE
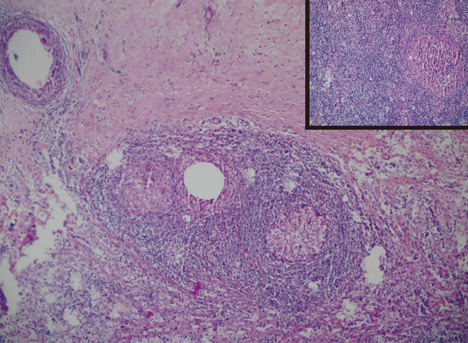
Idiopathic granulomatous lobular mastitis (IGLM) is a rare chronic inflammatory disease of the breast with obscure etiology that mimics invasive carcinoma both clinically and radiologically. The treatment of IGLM remains controversial. The aim of proper management is to use a combination of medical and surgical treatment of this benign condition to achieve a good cosmetic result and low recurrence rate.
METHODS
A retrospective analysis of 19 patients with IGLM is performed based on the findings of clinical, radiological, and pathological examinations. The results of two treatments are presented: medical treatment with oral corticosteroids, and consecutive surgical excision after a follow-up period of 20 months (range, 6-75 months).
RESULTS
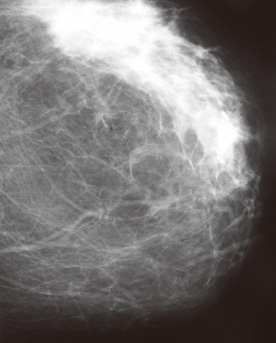
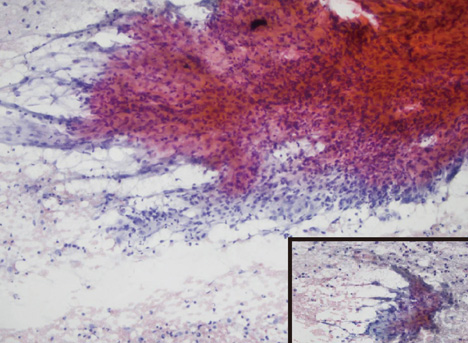
The majority of patients treated in this paper were young (mean, 34 years) parous women with a history of hormonal medication use. The main clinical finding is large, irregular, and painful mass. Hypoechoic lobulated, irregular tubular or oval shaped masses had been imaged by ultrasound. Mammographic findings were an ill-defined mass, enlarged axillary lymph nodes, asymmetric density, and architectural distortion. Diagnoses of IGLM had been established by cytological or histological examination. Symptoms subside and inflammatory changes regressed with medical treatment. The remaining lesions were excised by consecutive breast conserving surgery. The disease recurred in one patient during the follow-up period.
CONCLUSION
IGLM is an inflammatory breast disease found in young women who present with a large painful irregular mass, which mimics carcinoma, as a physical change. Breast imaging modalities are not helpful to differentiate IGLM from invasive cancer. The correct diagnosis is established by cytological or histological examination. Medical treatment with corticosteroids provides significant regression of the inflammatory disease, allowing more conservative surgery. Consecutive surgical excision of the remaining lesions with good cosmetic results provides definitive treatment and reduces the risk of recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Dixon JM, Bundred NJ. Harris JR, Lippman EM, Morrow M, Osborne CK, editors. Management of disorders of the ductal system and infections. Disease of the Breast. 2010. 4th ed. Philadelphia: Lippincott Williams & Wilkins;42–52.2. Al-Khaffaf B, Knox F, Bundred NJ. Idiopathic granulomatous mastitis: a 25-year experience. J Am Coll Surg. 2008. 206:269–273.
Article3. Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004. 10:318–322.
Article4. Lee JH, Oh KK, Kim EK, Kwack KS, Jung WH, Lee HK. Radiologic and clinical features of idiopathic granulomatous lobular mastitis mimicking advanced breast cancer. Yonsei Med J. 2006. 47:78–84.
Article5. Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K. Granulomatous mastitis: clinical, pathological features, and management. Breast J. 2010. 16:176–182.
Article6. Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, Igci A, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005. 11:108–114.
Article7. Kok KY, Telisinghe PU. Granulomatous mastitis: presentation, treatment and outcome in 43 patients. Surgeon. 2010. 8:197–201.
Article8. Erozgen F, Ersoy YE, Akaydin M, Memmi N, Celik AS, Celebi F, et al. Corticosteroid treatment and timing of surgery in idiopathic granulomatous mastitis confusing with breast carcinoma. Breast Cancer Res Treat. 2010. 123:447–452.
Article9. Tuli R, O'Hara BJ, Hines J, Rosenberg AL. Idiopathic granulomatous mastitis masquerading as carcinoma of the breast: a case report and review of the literature. Int Semin Surg Oncol. 2007. 4:21.
Article10. Bakaris S, Yuksel M, Ciragil P, Guven MA, Ezberci F, Bulbuloglu E. Granulomatous mastitis including breast tuberculosis and idiopathic lobular granulomatous mastitis. Can J Surg. 2006. 49:427–430.11. Memis A, Bilgen I, Ustun EE, Ozdemir N, Erhan Y, Kapkac M. Granulomatous mastitis: imaging findings with histopathologic correlation. Clin Radiol. 2002. 57:1001–1006.
Article12. Gupta RK. Fine needle aspiration cytology of granulomatous mastitis: a study of 18 cases. Acta Cytol. 2010. 54:138–141.13. Vinayagam R, Cox J, Webb L. Granulomatous mastitis: a spectrum of disease. Breast Care (Basel). 2009. 4:251–254.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Topical Steroids to Treat Granulomatous Mastitis: A Case Report
- Surgical Treatment for Idiopathic Granulomatous Mastitis
- Granulomatous Mastitis during Chronic Antidepressant Therapy: Is It Possible a Conservative Therapeutic Approach?
- Nodular Metastatic Carcinoma from Invasive Lobular Breast Cancer
- Erythema Nodosum Associated with Idiopathic Granulomatous Mastitis in Young Pregnant Woman