J Breast Cancer.
2012 Mar;15(1):91-97. 10.4048/jbc.2012.15.1.91.
The Efficacy of Arm Node Preserving Surgery Using Axillary Reverse Mapping for Preventing Lymphedema in Patients with Breast Cancer
- Affiliations
-
- 1Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea. crystallee@med.yu.ac.kr
- 2Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2286479
- DOI: http://doi.org/10.4048/jbc.2012.15.1.91
Abstract
- PURPOSE
The axillary reverse mapping (ARM) technique to identify and preserve arm nodes during sentinel lymph node biopsy (SLNB) or axillary lymph node dissection (ALND) was developed to prevent lymphedema. The purpose of this study was to investigate the location and metastatic rate of the arm node, and to evaluate the short term incidence of lymphedema after arm node preserving surgery.
METHODS
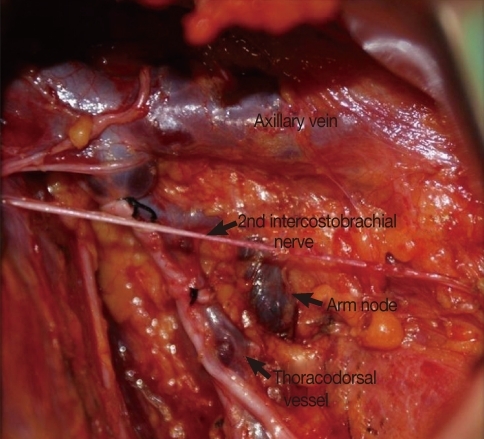
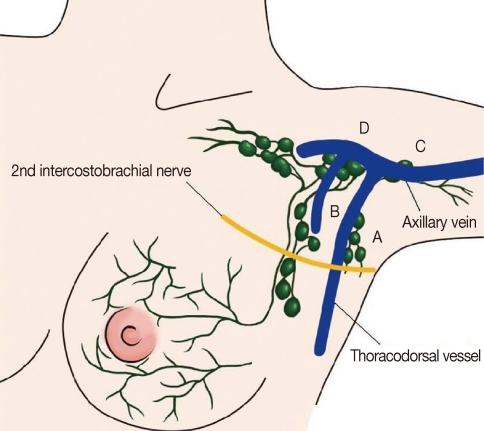
From January 2009 to October 2010, 97 breast cancer patients who underwent ARM were included. Blue-dye (2.5 mL) was injected into the ipsilateral upper-inner arm. At least 20 minutes after injection, SLNB or ALND was performed and blue-stained arm nodes and/or lymphatics were identified. Patients were divided into two groups, an arm node preserved group (70 patients had ALND, 10 patients had SLNB) and an unpreserved group (13 patients had ALND, 4 patients had SLNB). The difference in arm circumference between preoperative and postoperative time points was checked in both groups.
RESULTS
The mean number of identified blue stained arm nodes was 1.4+/-0.6. In the majority of patients (92%), arm nodes were located between the lower level of the axillary vein and just below the second intercostobrachial nerve. In the arm node unpreserved group, 2 patients had metastasis in their arm node. Among ALND patients, in the arm node preserved group, the difference in arm circumference between preoperative and postoperative time points in ipsilateral and contralateral arms was 0.27 cm and 0.07 cm, respectively, whereas it was 0.47 cm and -0.03 cm in the unpreserved group; one case of lymphedema was found after 6 months. No difference was found between arm node preserved and unpreserved group among SLNB patients.
CONCLUSION
Arm node preserving was possible in all breast cancer patients with identifiable arm nodes, during ALND or SLNB, except for those with high surgical N stage, and lymphedema did not develop in patients with arm node preserving surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Petrek JA, Senie RT, Peters M, Rosen PP. Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer. 2001; 92:1368–1377. PMID: 11745212.
Article2. Ivens D, Hoe AL, Podd TJ, Hamilton CR, Taylor I, Royle GT. Assessment of morbidity from complete axillary dissection. Br J Cancer. 1992; 66:136–138. PMID: 1637663.
Article3. Newman ML, Brennan M, Passik S. Lymphedema complicated by pain and psychological distress: a case with complex treatment needs. J Pain Symptom Manage. 1996; 12:376–379. PMID: 8973048.
Article4. Schrenk P, Rieger R, Shamiyeh A, Wayand W. Morbidity following sentinel lymph node biopsy versus axillary lymph node dissection for patients with breast carcinoma. Cancer. 2000; 88:608–614. PMID: 10649254.
Article5. Sener SF, Winchester DJ, Martz CH, Feldman JL, Cavanaugh JA, Winchester DP, et al. Lymphedema after sentinel lymphadenectomy for breast carcinoma. Cancer. 2001; 92:748–752. PMID: 11550143.
Article6. Wilke LG, McCall LM, Posther KE, Whitworth PW, Reintgen DS, Leitch AM, et al. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol. 2006; 13:491–500. PMID: 16514477.
Article7. Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S, Westbrook KC, et al. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol. 2007; 14:1890–1895. PMID: 17479341.
Article8. Nos C, Lesieur B, Clough KB, Lecuru F. Blue dye injection in the arm in order to conserve the lymphatic drainage of the arm in breast cancer patients requiring an axillary dissection. Ann Surg Oncol. 2007; 14:2490–2496. PMID: 17549570.
Article9. Britton TB, Solanki CK, Pinder SE, Mortimer PS, Peters AM, Purushotham AD. Lymphatic drainage pathways of the breast and the upper limb. Nucl Med Commun. 2009; 30:427–430. PMID: 19319006.
Article10. Choi JE, Jeon YS, Kang SH, Lee SJ. Preservation of lymphatic drainage of arm during axillary procedure in breast cancer patients. J Breast Cancer. 2009; 12:179–185.
Article11. Nos C, Kaufmann G, Clough KB, Collignon MA, Zerbib E, Cusumano P, et al. Combined axillary reverse mapping (ARM) technique for breast cancer patients requiring axillary dissection. Ann Surg Oncol. 2008; 15:2550–2555. PMID: 18618185.
Article12. McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008; 26:5213–5219. PMID: 18838709.
Article13. Bedrosian I, Babiera GV, Mittendorf EA, Kuerer HM, Pantoja L, Hunt KK, et al. A phase I study to assess the feasibility and oncologic safety of axillary reverse mapping in breast cancer patients. Cancer. 2010; 116:2543–2548. PMID: 20336790.
Article14. Noguchi M, Yokoi M, Nakano Y. Axillary reverse mapping with indocyanine fluorescence imaging in patients with breast cancer. J Surg Oncol. 2010; 101:217–221. PMID: 20063370.
Article15. Noguchi M. Axillary reverse mapping for breast cancer. Breast Cancer Res Treat. 2010; 119:529–535. PMID: 19842033.
Article16. Casabona F, Bogliolo S, Valenzano Menada M, Sala P, Villa G, Ferrero S. Feasibility of axillary reverse mapping during sentinel lymph node biopsy in breast cancer patients. Ann Surg Oncol. 2009; 16:2459–2463. PMID: 19506954.
Article17. Ponzone R, Mininanni P, Cassina E, Sismondi P. Axillary reverse mapping in breast cancer: can we spare what we find? Ann Surg Oncol. 2008; 15:390–391. PMID: 17990039.
Article18. Boneti C, Korourian S, Diaz Z, Santiago C, Mumford S, Adkins L, et al. Scientific Impact Award: axillary reverse mapping (ARM) to identify and protect lymphatics draining the arm during axillary lymphadenectomy. Am J Surg. 2009; 198:482–487. PMID: 19800452.
Article19. Peter C, Hongwan D, Küpfer A, Lauterburg BH. Pharmacokinetics and organ distribution of intravenous and oral methylene blue. Eur J Clin Pharmacol. 2000; 56:247–250. PMID: 10952480.
Article20. Walter-Sack I, Rengelshausen J, Oberwittler H, Burhenne J, Mueller O, Meissner P, et al. High absolute bioavailability of methylene blue given as an aqueous oral formulation. Eur J Clin Pharmacol. 2009; 65:179–189. PMID: 18810398.
Article21. Boneti C, Korourian S, Bland K, Cox K, Adkins LL, Henry-Tillman RS, et al. Axillary reverse mapping: mapping and preserving arm lymphatics may be important in preventing lymphedema during sentinel lymph node biopsy. J Am Coll Surg. 2008; 206:1038–1042. PMID: 18471751.
Article22. Deutsch M, Land S, Begovic M, Sharif S. The incidence of arm edema in women with breast cancer randomized on the National Surgical Adjuvant Breast and Bowel Project study B-04 to radical mastectomy versus total mastectomy and radiotherapy versus total mastectomy alone. Int J Radiat Oncol Biol Phys. 2008; 70:1020–1024. PMID: 18029105.
Article23. Gartner R, Jensen MB, Kronborg L, Ewertz M, Kehlet H, Kroman N. Self-reported arm-lymphedema and functional impairment after breast cancer treatment: a nationwide study of prevalence and associated factors. Breast. 2010; 19:506–515. PMID: 20561790.24. Ward LC. Bioelectrical impedance analysis: proven utility in lymphedema risk assessment and therapeutic monitoring. Lymphat Res Biol. 2006; 4:51–56. PMID: 16569209.
Article25. Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR. Validation of an optoelectronic limb volumeter (Perometer). Lymphology. 1997; 30:77–97. PMID: 9215977.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arm Sentinel Lymph Node Detection for Preserving the Arm Lymphatic System
- Preservation of Lymphatic Drainage of Arm during Axillary Procedure in Breast Cancer Patients
- Effects of Education Program for Combined Management of Lymphedema with regard to Breast Cancer Patients with Axillary Lymph Node Dissection: A Quasi-Experimental Study
- Six-Month Follow-up for Investigating the Effect of Prophylactic Lymphovenous Anastomosis on the Prevention of Breast Cancer-Related Lymphedema: A Preliminary Study in a Single Institution
- Rapid Lymphedema Progression in Breast Cancer Patient with Previous Forearm Fracture