J Breast Cancer.
2012 Dec;15(4):434-440. 10.4048/jbc.2012.15.4.434.
The Relationship between Surgery and Phase of the Menstrual Cycle Affects Survival in Breast Cancer
- Affiliations
-
- 1Department of General Surgery, Ankara Oncology Hospital, Ankara, Turkey. atalay_can@hotmail.com
- KMID: 2286441
- DOI: http://doi.org/10.4048/jbc.2012.15.4.434
Abstract
- PURPOSE
The impact of time of surgery based on the menstrual cycle is a controversial issue. Two decades after the first interest in this topic, a number of studies with conflicting results have not helped to resolve this problem. This study aimed to prospectively evaluate the impact of timing of surgery based on the menstrual cycle on survival rates of breast cancer patients, and various clinical and hormonal classifications of the menstrual cycle were compared in order to determine the phase of the menstrual cycle which showed the highest degree of surgical survival.
METHODS
Premenopausal breast cancer patients treated with curative surgery between 1998 and 2002 were prospectively included in this study. Patients were divided into different groups according to the first day of their last menstrual cycle using three different classifications (clinical, Hrushesky, Badwe), and were also grouped according to their serum hormone levels. Serum levels of follicle stimulating hormone, luteinizing hormone, estrogen, and progesterone were measured on the day of surgery.
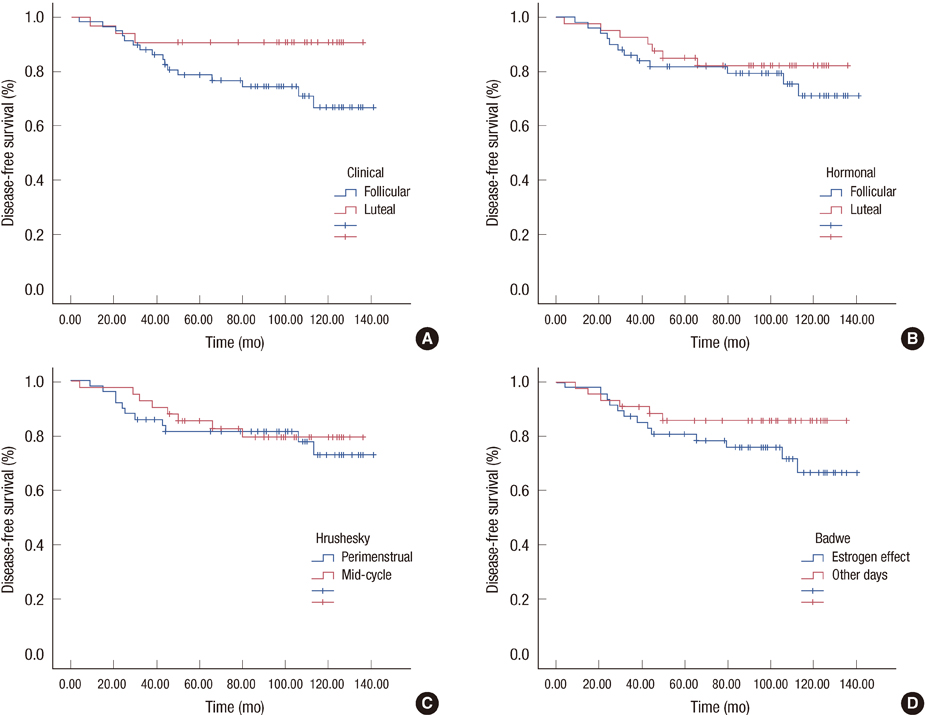
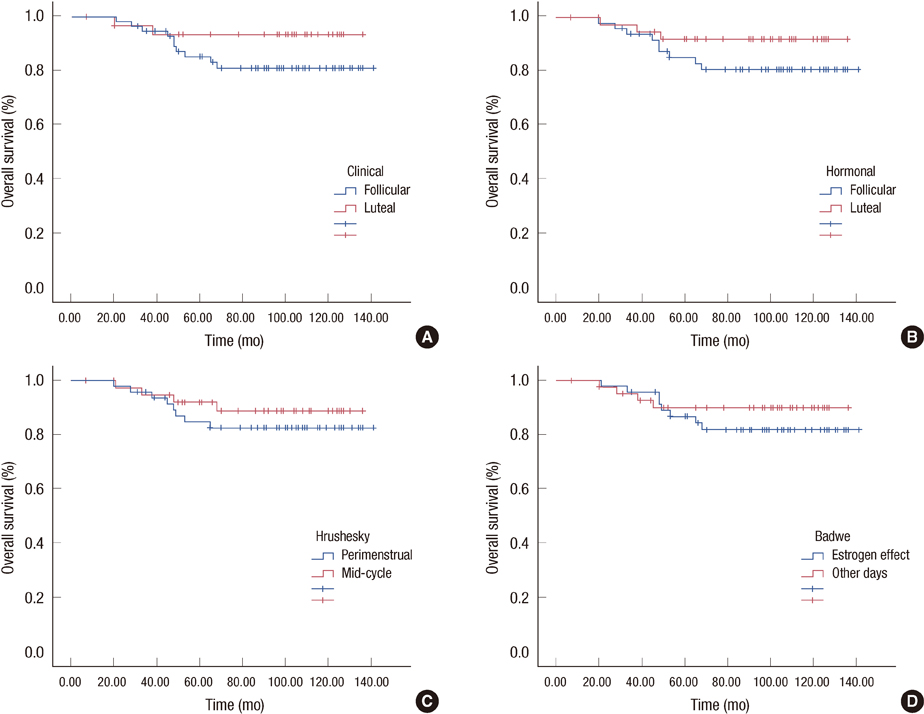
RESULTS
Ninety patients were included in the study. Median follow-up time was 90 months. Nineteen patients (21.1%) had loco-regional recurrence and/or distant metastases while 12 patients (13.3%) died during follow-up. Five-year (78.6% vs. 90.6%) and 10-year (66.7% vs. 90.6%) disease-free survival (DFS) rates of patients in the clinically defined follicular phase were significantly decreased compared to luteal phase. On the other hand, hormonally determined phases of the menstrual cycle and grouping of patients according to clinical classifications did not show an impact on prognosis.
CONCLUSION
In the current study performing surgery in the follicular phase of the menstrual cycle decreased DFS in premenopausal patients. According to these results, performing surgery during the luteal phase of the menstrual cycle might have a beneficial effect on survival.
Keyword
MeSH Terms
-
Breast
Breast Neoplasms
Disease-Free Survival
Estrogens
Female
Follicle Stimulating Hormone
Follicular Phase
Follow-Up Studies
Hand
Humans
Luteal Phase
Luteinizing Hormone
Menstrual Cycle
Neoplasm Metastasis
Progesterone
Prospective Studies
Recurrence
Survival Rate
Estrogens
Follicle Stimulating Hormone
Luteinizing Hormone
Progesterone
Figure
Reference
-
1. Kroman N. Timing of breast cancer surgery in relation to the menstrual cycle: the rise and fall of a hypothesis. Acta Oncol. 2008. 47:576–579.
Article2. Hrushesky WJ, Bluming AZ, Gruber SA, Sothern RB. Menstrual influence on surgical cure of breast cancer. Lancet. 1989. 2:949–952.
Article3. Senie RT, Rosen PP, Rhodes P, Lesser ML. Timing of breast cancer excision during the menstrual cycle influences duration of disease-free survival. Ann Intern Med. 1991. 115:337–342.
Article4. Badwe RA, Gregory WM, Chaudary MA, Richards MA, Bentley AE, Rubens RD, et al. Timing of surgery during menstrual cycle and survival of premenopausal women with operable breast cancer. Lancet. 1991. 337:1261–1264.
Article5. Saad Z, Bramwell V, Duff J, Girotti M, Jory T, Heathcote G, et al. Timing of surgery in relation to the menstrual cycle in premenopausal women with operable breast cancer. Br J Surg. 1994. 81:217–220.
Article6. Saad Z, Vincent M, Bramwell V, Stitt L, Duff J, Girotti M, et al. Timing of surgery influences survival in receptor-negative as well as receptor-positive breast cancer. Eur J Cancer. 1994. 30A:1348–1352.
Article7. Hagen AA, Hrushesky WJ. Menstrual timing of breast cancer surgery. Am J Surg. 1998. 175:245–261.8. Veronesi U, Luini A, Mariani L, Del Vecchio M, Alvez D, Andreoli C, et al. Effect of menstrual phase on surgical treatment of breast cancer. Lancet. 1994. 343:1545–1547.
Article9. Pujol P, Daures JP, Brouillet JP, Chang S, Rouanet P, Bringer J, et al. A prospective prognostic study of the hormonal milieu at the time of surgery in premenopausal breast carcinoma. Cancer. 2001. 91:1854–1861.
Article10. Kroman N, Højgaard A, Andersen KW, Graversen HP, Afzelius P, Lokdam A, et al. Danish Breast Cancer Cooperative Group. Timing of surgery in relation to menstrual cycle does not predict the prognosis in primary breast cancer. Eur J Surg Oncol. 1994. 20:430–435.
Article11. Love RR, Duc NB, Dinh NV, Shen TZ, Havighurst TC, Allred DC, et al. Mastectomy and oophorectomy by menstrual cycle phase in women with operable breast cancer. J Natl Cancer Inst. 2002. 94:662–669.
Article12. Goldhirsch A, Gelber RD, Castiglione M, O'Neill A, Thürlimann B, Rudenstam CM, et al. Menstrual cycle and timing of breast surgery in premenopausal node-positive breast cancer: results of the International Breast Cancer Study Group (IBCSG) Trial VI. Ann Oncol. 1997. 8:751–756.
Article13. Badwe RA, Wang DY, Gregory WM, Fentiman IS, Chaudary MA, Smith P, et al. Serum progesterone at the time of surgery and survival in women with premenopausal operable breast cancer. Eur J Cancer. 1994. 30A:445–448.
Article14. Goldfarb Y, Ben-Eliyahu S. Surgery as a risk factor for breast cancer recurrence and metastasis: mediating mechanisms and clinical prophylactic approaches. Breast Dis. 2006. 26:99–114.
Article15. Chaudhry A, Puntis ML, Gikas P, Mokbel K. Does the timing of breast cancer surgery in pre-menopausal women affect clinical outcome? An update. Int Semin Surg Oncol. 2006. 3:37.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Menstruation and Sleep
- Influence of the Phase of Menstrual Cycle on Postoperative Nausea and Vomiting after Breast Cancer Surgery
- Effect of the Menstrual Cycle on Background Parenchymal Enhancement Observed on Breast MRIs in Korean Women
- Sustainable Rates of Sebum Excretion in Relation to Menstrual Cycle
- Telomerase Activity in Endometrium According to Menstrual Cycle