J Breast Cancer.
2013 Sep;16(3):274-284. 10.4048/jbc.2013.16.3.274.
Prognostic Value of the Nodal Ratio and Ki-67 Expression in Breast Cancer Patients Treated with Postmastectomy Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. inah228@snu.ac.kr
- 2Breast Care Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2286378
- DOI: http://doi.org/10.4048/jbc.2013.16.3.274
Abstract
- PURPOSE
This pilot study aimed to evaluate prognostic factors of postmastectomy radiotherapy (PMRT) for breast cancer patients undergoing systemic therapy in either preoperative or postoperative setting.
METHODS
Between 2003 and 2009, 113 patients received PMRT: 61 underwent preoperative systemic therapy (PST subgroup) and 52 received postoperative systemic therapy (non-PST subgroup).
RESULTS
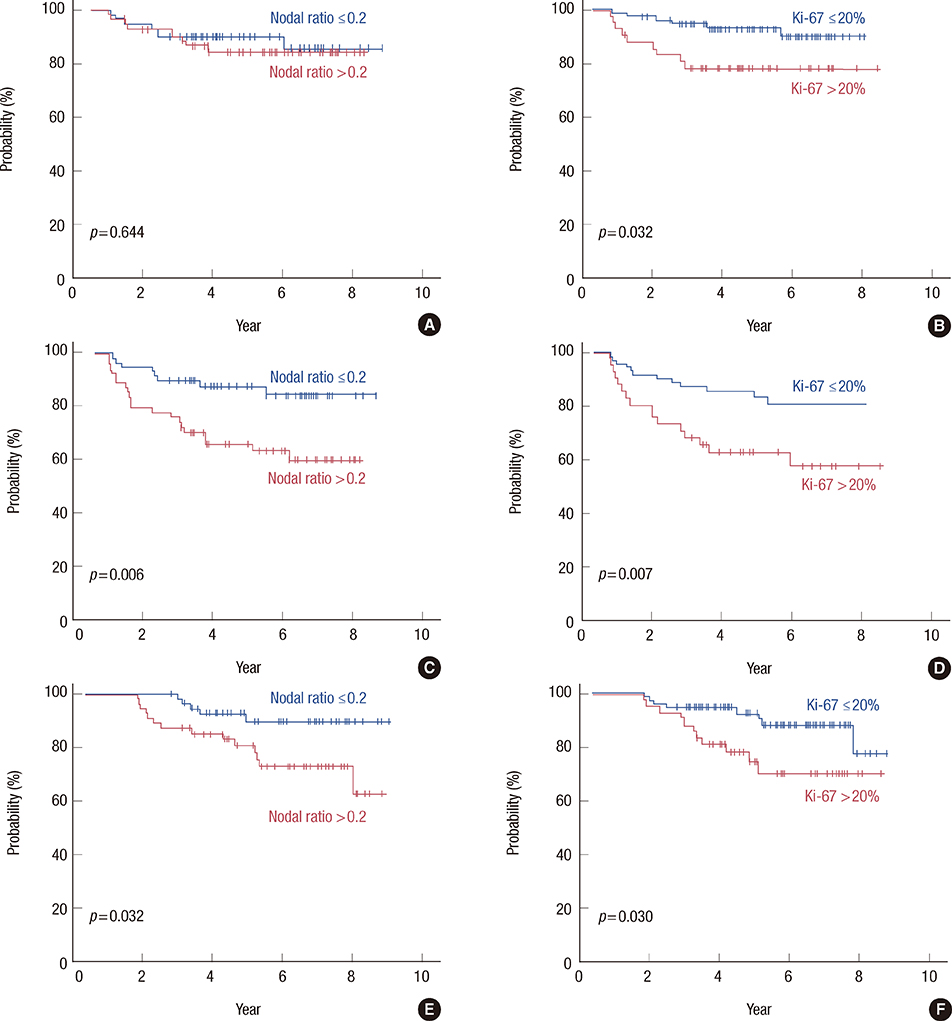
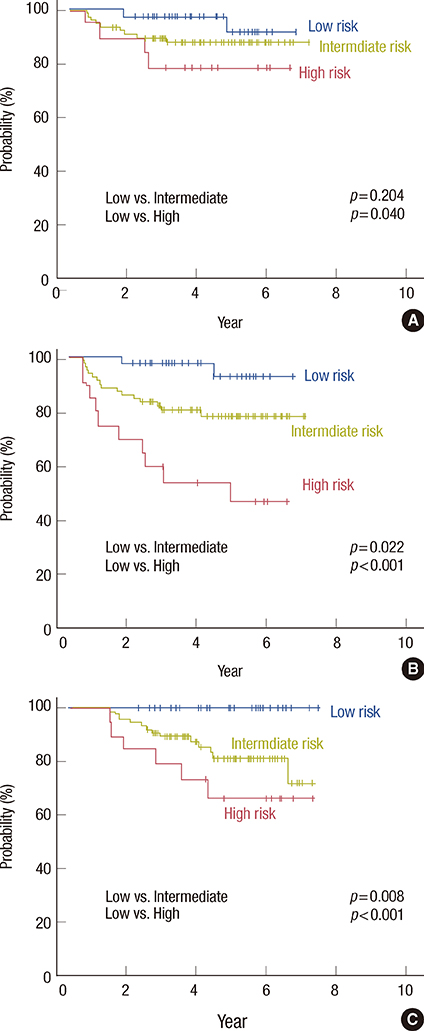
The median follow-up time was 72.3 months (range, 34.0-109.4 months) for surviving patients. In univariate analysis of all patients, disease-free survival (DFS) was associated with age, nodal ratio (NR), and Ki-67 expression; overall survival (OS) was associated with NR and Ki-67 expression. Pathologic N stage and HER2 expression were marginally associated with DFS and OS. In the non-PST subgroup, DFS was associated with age, NR, venous invasion, and Ki-67 expression; OS was associated with age. In the PST subgroup, DFS was associated with ypN stage and NR; OS was associated with ypN, histologic grade, HER2 expression, and p53 expression. In multivariate analysis of all patients, DFS and OS were significantly associated with NR (p=0.003 and p=0.019, respectively) and Ki-67 expression (p=0.002 and p=0.015, respectively). Patients were classified into low-risk (NR < or =0.2 and Ki-67 < or =20%; n=34), intermediate-risk (NR >0.2 or Ki-67 >20%; n=63), and high-risk (NR >0.2 and Ki-67 >20%; n=16) subgroups. All low-risk patients were alive at the time of analysis. High-risk (p<0.001 and p=0.001, respectively) and intermediate-risk (p=0.022 and p=0.008, respectively) patients had significantly shorter DFS and OS than low-risk patients. This prognostic model was statistically significant for DFS when applied to the PST (p=0.001) and non-PST (p=0.016) subgroups separately.
CONCLUSION
For breast cancer patients undergoing PMRT, NR and Ki-67 are potential prognostic factors. A model using these factors might help predict a poor prognosis. Whether NR and Ki-67 are also prognostic for different setting of systemic therapy, preoperative or postoperative, warrants further study.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Prognostic Model for Patients with Triple-Negative Breast Cancer: Importance of the Modified Nottingham Prognostic Index and Age
Jeanny Kwon, Keun-Yong Eom, Tae Ryool Koo, Byoung Hyuck Kim, Eunyoung Kang, Sung-Won Kim, Yu Jung Kim, So Yeon Park, In Ah Kim
J Breast Cancer. 2017;20(1):65-73. doi: 10.4048/jbc.2017.20.1.65.
Reference
-
1. Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997; 337:949–955.
Article2. Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999; 353:1641–1648.
Article3. Ragaz J, Olivotto IA, Spinelli JJ, Phillips N, Jackson SM, Wilson KS, et al. Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst. 2005; 97:116–126.
Article4. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. American Joint Committee on Cancer. AJCC Cancer Staging Manual. 7th ed. New York: Springer;2010.5. Han TJ, Kang EY, Jeon W, Kim SW, Kim JH, Kim YJ, et al. The prognostic value of the nodal ratio in N1 breast cancer. Radiat Oncol. 2011; 6:131.
Article6. Keam B, Im SA, Kim HJ, Oh DY, Kim JH, Lee SH, et al. Clinical significance of axillary nodal ratio in stage II/III breast cancer treated with neoadjuvant chemotherapy. Breast Cancer Res Treat. 2009; 116:153–160.
Article7. Vinh-Hung V, Verkooijen HM, Fioretta G, Neyroud-Caspar I, Rapiti E, Vlastos G, et al. Lymph node ratio as an alternative to pN staging in node-positive breast cancer. J Clin Oncol. 2009; 27:1062–1068.
Article8. Truong PT, Berthelet E, Lee J, Kader HA, Olivotto IA. The prognostic significance of the percentage of positive/dissected axillary lymph nodes in breast cancer recurrence and survival in patients with one to three positive axillary lymph nodes. Cancer. 2005; 103:2006–2014.
Article9. Truong PT, Woodward WA, Thames HD, Ragaz J, Olivotto IA, Buchholz TA. The ratio of positive to excised nodes identifies high-risk subsets and reduces inter-institutional differences in locoregional recurrence risk estimates in breast cancer patients with 1-3 positive nodes: an analysis of prospective data from British Columbia and the M. D. Anderson Cancer Center. Int J Radiat Oncol Biol Phys. 2007; 68:59–65.
Article10. Ahn SH, Kim HJ, Lee JW, Gong GY, Noh DY, Yang JH, et al. Lymph node ratio and pN staging in patients with node-positive breast cancer: a report from the Korean Breast Cancer Society. Breast Cancer Res Treat. 2011; 130:507–515.
Article11. Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ. Panel members. Strategies for subtypes--dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011; 22:1736–1747.
Article12. Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009; 101:736–750.
Article13. Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010; 28:1684–1691.
Article14. de Azambuja E, Cardoso F, de Castro G Jr, Colozza M, Mano MS, Durbecq V, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer. 2007; 96:1504–1513.
Article15. Jones RL, Salter J, A'Hern R, Nerurkar A, Parton M, Reis-Filho JS, et al. The prognostic significance of Ki67 before and after neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat. 2009; 116:53–68.
Article16. Selz J, Stevens D, Jouanneau L, Labib A, Le Scodan R. Prognostic value of molecular subtypes, Ki67 expression and impact of postmastectomy radiation therapy in breast cancer patients with negative lymph nodes after mastectomy. Int J Radiat Oncol Biol Phys. 2012; 84:1123–1132.
Article17. Jang MH, Kim EJ, Choi Y, Lee HE, Kim YJ, Kim JH, et al. FGFR1 is amplified during the progression of in situ to invasive breast carcinoma. Breast Cancer Res. 2012; 14:R115.18. Hammond ME, Hayes DF, Wolff AC. Clinical Notice for American Society of Clinical Oncology-College of American Pathologists guideline recommendations on ER/PgR and HER2 testing in breast cancer. J Clin Oncol. 2011; 29:e458.
Article19. Overgaard M, Nielsen HM, Overgaard J. Is the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trials. Radiother Oncol. 2007; 82:247–253.
Article20. Schmoor C, Sauerbrei W, Bastert G, Bojar H, Schumacher M. German Breast Cancer Study Group. Long-term prognosis of breast cancer patients with 10 or more positive lymph nodes treated with CMF. Eur J Cancer. 2001; 37:1123–1131.
Article21. Woodward WA, Vinh-Hung V, Ueno NT, Cheng YC, Royce M, Tai P, et al. Prognostic value of nodal ratios in node-positive breast cancer. J Clin Oncol. 2006; 24:2910–2916.
Article22. Canadian Association of Radiation Oncologists; The Steering Committee on Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Axillary dissection. CMAJ. 1998; 158:Suppl 3. S22–S26.23. Katz A, Buchholz TA, Thames H, Smith CD, McNeese MD, Theriault R, et al. Recursive partitioning analysis of locoregional recurrence patterns following mastectomy: implications for adjuvant irradiation. Int J Radiat Oncol Biol Phys. 2001; 50:397–403.
Article24. Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, et al. Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003; 56:658–670.
Article25. Wai ES, Lesperance M, Speers CH, Truong PT, Jones S, Tyldesley S, et al. Increased use of regional radiotherapy is associated with improved outcome in a population-based cohort of women with breast cancer with 1-3 positive nodes. Radiother Oncol. 2010; 97:301–306.
Article26. Truong PT, Jones SO, Kader HA, Wai ES, Speers CH, Alexander AS, et al. Patients with t1 to t2 breast cancer with one to three positive nodes have higher local and regional recurrence risks compared with node-negative patients after breast-conserving surgery and whole-breast radiotherapy. Int J Radiat Oncol Biol Phys. 2009; 73:357–364.
Article27. Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004; 351:2817–2826.
Article28. Viale G, Giobbie-Hurder A, Regan MM, Coates AS, Mastropasqua MG, Dell'Orto P, et al. Prognostic and predictive value of centrally reviewed Ki-67 labeling index in postmenopausal women with endocrine-responsive breast cancer: results from Breast International Group Trial 1-98 comparing adjuvant tamoxifen with letrozole. J Clin Oncol. 2008; 26:5569–5575.
Article29. Yerushalmi R, Woods R, Ravdin PM, Hayes MM, Gelmon KA. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol. 2010; 11:174–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prognostic Value of the S-phase Fraction and Ki-67 Expression in Early Breast Cancer
- Usefulness of Ki-67 as a prognostic factor in lymph node-negative breast cancer
- Postmastectomy Radiation Therapy in Patients With Minimally Involved Lymph Nodes: A Review of the Current Data and Future Directions
- Leptin and Leptin Receptor Expression in Breast Cancer
- Expression of Topoisomerase II alpha and Ki-67 in Invasive Mammary Carcinoma and Their Clinicopathologic Implication