Infect Chemother.
2013 Jun;45(2):194-201. 10.3947/ic.2013.45.2.194.
Blood Stream Infections in Patients in the Burn Intensive Care Unit
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea. infwoo@hallym.or.kr
- 2Burn Plastic Surgery Center, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea.
- 3Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2285000
- DOI: http://doi.org/10.3947/ic.2013.45.2.194
Abstract
- BACKGROUND
The study on bacteremia helps empirically select the proper antibiotics before the results of culture test about causative pathogen. The purpose of this study is to investigate causative pathogen in bloodstream infection, changing aspects based on elapsed time after burn, relationship with other sites and resistance of important causative pathogen against antibiotics through analysis on bacteria isolated from blood culture of patients hospitalized in burn intensive care unit (BICU).
MATERIALS AND METHODS
A retrospective study was conducted targeting patients hospitalized in BICU from January 2007 to June 2011. Changes of causative pathogen in bloodstream infection based on elapsed time after injury were analyzed. We would like to examine the relationship between bloodstream infection and infection on other body parts by comparing results of cultures in burn wound site, sputum, urine and catheter tip. Antibiotics resistance patterns of Pseudomonas aeruginosa, Acinetobacter baumannii, Staphylococcus aureus, Enterococcus species, and Klebsiella pneumoniae were studied.
RESULTS
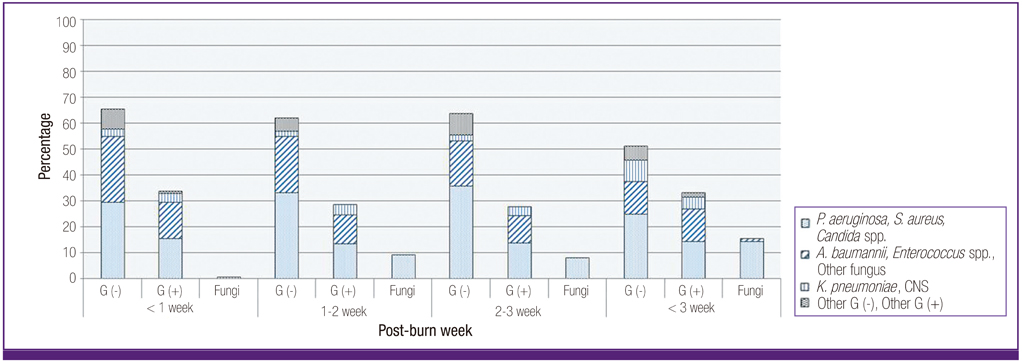
A total of 2,337 burn patients were hospitalized in BICU for 54 months. Causative pathogen was cultured in blood cultures from 397 patients (17.0%). P. aeruginosa (169, 30.1%) was the most cultured and A. baumannii (107, 19.0%) and S. aureus (81, 14.4%) were followed. It was confirmed that the relative frequency of A. baumannii tended to get lower as the period got longer after injury, but the relative frequency of K. pneumoniae got higher as the period got longer after injury. With comparison without bacteremia, P. aeruginosa bacteremia showed high probability in which the same bacteria were cultured in wound site, sputum and cathether tip, and A. baumannii bacteremia and candida bacteremia had high probability in sputum, and urine and catheter tip, respectively. 95.9% of P. aeruginosa and 95.3% of A. baumannii showed the resistance against carbapenem. 96.3% of S. aureus was methicillin resistant and 36.2% of Enterococcus species were vancomycin resistant. 75.0% of K. pneumonia were extended-spectrum beta-lactamase (ESBL)-producing bacteria.
CONCLUSIONS
Since the highly antibiotic resistant microorganisms were isolated from the patients hospitalized in BICU during early phase, the empirical selection of antibiotics targeting these pathogens should be considered before the results of microbiologic culture test. In addition, use of empirical antifungal agent after 1 week of injury can be considered for patients who have risk factor of fungal infection.
Keyword
MeSH Terms
-
Acinetobacter baumannii
Anti-Bacterial Agents
Bacteremia
Bacteria
beta-Lactamases
Burns
Candida
Catheters
Critical Care
Enterococcus
Human Body
Humans
Intensive Care Units
Klebsiella pneumoniae
Methicillin Resistance
Pneumonia
Pseudomonas aeruginosa
Retrospective Studies
Risk Factors
Rivers
Sputum
Staphylococcus aureus
Vancomycin
Anti-Bacterial Agents
Vancomycin
beta-Lactamases
Figure
Reference
-
1. Lari AR, Alaghehbandan R. Nosocomial infections in an Iranian burn care center. Burns. 2000. 26:737–740.
Article2. Weber J, McManus A. Nursing Committee of the International Society for Burn Injuries. Infection control in burn patients. Burns. 2004. 30:A16–A24.
Article3. Altoparlak U, Erol S, Akcay MN, Celebi F, Kadanali A. The time-related changes of antimicrobial resistance patterns and predominant bacterial profiles of burn wounds and body flora of burned patients. Burns. 2004. 30:660–664.
Article4. Suljagic V, Jevtic M, Djordjevic B, Romic P, Ilic R, Stankovic N, Milovic N, Novakovic M, Kozarski J, Roganovic Z, Popovic Z, Jovelic A. Epidemiology of nosocomial colonization/infection caused by Acinetobacter spp. in patients of six surgical clinics in war and peacetime. Vojnosanit Pregl. 2011. 68:661–668.
Article5. Henwood CJ, Livermore DM, Johnson AP, James D, Warner M, Gardiner A. The Linezolid Study Group. Susceptibility of gram-positive cocci from 25 UK hospitals to antimicrobial agents including linezolid. J Antimicrob Chemother. 2000. 46:931–940.
Article6. Chong SJ, Ahmed S, Tay JM, Song C, Tan TT. 5 year analysis of bacteriology culture in a tropical burns ICU. Burns. 2011. 37:1349–1353.
Article7. Vostrugina K, Gudaviciene D, Vitkauskiene A. Bacteremias in patients with severe burn trauma. Medicina (Kaunas). 2006. 42(7):576–579.8. Gang RK, Sanyal SC, Bang RL, Mokaddas E, Lari AR. Staphylococcal septicaemia in burns. Burns. 2000. 26:359–366.
Article9. Still J, Law E, Friedman B, Fuhrman S, Newton T. Vancomycin-resistant organisms on a burn unit. South Med J. 2001. 94:810–812.
Article10. Nasser S, Mabrouk A, Maher A. Colonization of burn wounds in Ain Shams University Burn Unit. Burns. 2003. 29:229–233.
Article11. Vindenes H, Bjerknes R. Microbial colonization of large wounds. Burns. 1995. 21:575–579.
Article12. Pedrosa AF, Rodrigues AG. Candidemia in burn patients: figures and facts. J Trauma. 2011. 70:498–506.
Article13. Ballard J, Edelman L, Saffle J, Sheridan R, Kagan R, Bracco D, Cancio L, Cairns B, Baker R, Fillari P, Wibbenmeyer L, Voight D, Palmieri T, Greenhalgh D, Kemalyan N, Caruso D. Multicenter Trials Group, American Burn Association. Positive fungal cultures in burn patients: a multicenter review. J Burn Care Res. 2008. 29:213–221.
Article14. Ozkurt Z, Ertek M, Erol S, Altoparlak U, Akcay MN. The risk factors for acquisition of imipenem-resistant Pseudomonas aeruginosa in the burn unit. Burns. 2005. 31:870–873.
Article15. Trottier V, Segura PG, Namias N, King D, Pizano LR, Schulman CI. Outcomes of Acinetobacter baumannii infection in critically ill burned patients. J Burn Care Res. 2007. 28:248–254.
Article16. Levin AS, Barone AA, Penço J, Santos MV, Marinho IS, Arruda EA, Manrique EI, Costa SF. Intravenous colistin as therapy for nosocomial infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Clin Infect Dis. 1999. 28:1008–1011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nosocomial Infections in Intensive Care Unit: Epidemiology and Control Strategy
- Herpes Zoster Manifestation in the Treatment of a Facial Scald Burn: A Case Report
- Central Venous Catheter-related Infection in Major Burn Patients: Comparison of Subclavian Vein and Femoral Vein
- Analysis of Death of Burn Patients in a Burn Specialized Hospital: A Retrospective Clinical Study
- Predictive Factors of Intensive Care Unit Readmission among Older Patients: A Retrospective Study