Intest Res.
2015 Apr;13(2):153-159. 10.5217/ir.2015.13.2.153.
Patient Descriptions of Rectal Effluents May Help to Predict the Quality of Bowel Preparation With Photographic Examples
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhyang@amc.seoul.kr
- 2Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 3Department of Applied Statistics, Gachon University, Seongnam, Korea. hanseungbong@gachon.ac.kr
- KMID: 2284882
- DOI: http://doi.org/10.5217/ir.2015.13.2.153
Abstract
- BACKGROUND/AIMS
Previous studies have suggested a weak correlation between self-reported rectal effluent status and bowel preparation quality. We aim to evaluate whether photographic examples of rectal effluents could improve the correlation between patient descriptions of rectal effluents and bowel preparation quality.
METHODS
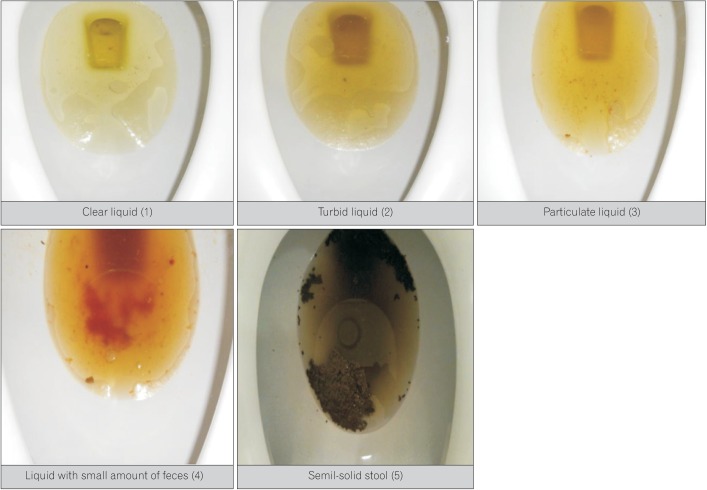
Before colonoscopy, patients were asked to describe the nature of their last three rectal effluents. Photographic examples of rectal effluents were provided as a reference for scoring. Bowel preparation was subsequently assessed by a single endoscopist using a global preparation assessment scale. Preparation outcomes were grouped into two levels (excellent to good vs. fair to inadequate). Both univariate and multivariate logistic regression models were used to find any association between bowel preparation quality and patient characteristics.
RESULTS
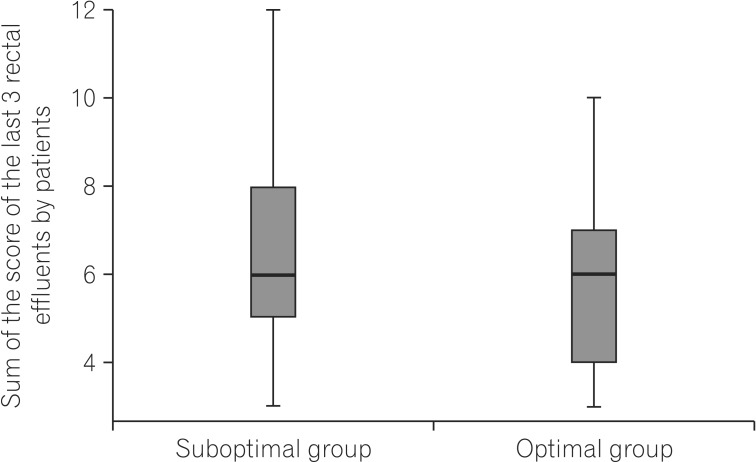
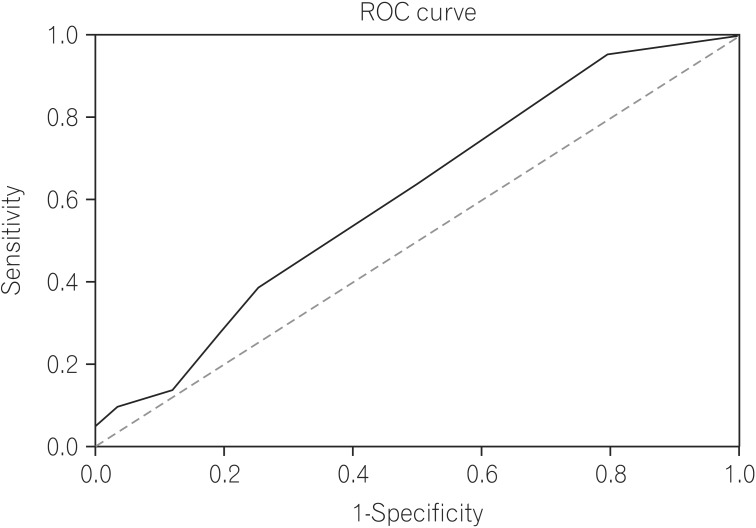
A total of 138 patients completed the questionnaires. The mean age was 56.5+/-10.4 years. The mean sum of the last three rectal effluent scores was 5.9+/-2.0. Higher rectal effluent scores (odds ratio [OR], 0.82; P=0.043) and the presence of diverticula (OR, 0.16; P<0.001) were risk factors for suboptimal preparation.
CONCLUSIONS
Photographic example-guided patient descriptions of rectal effluents showed a statistically significant association with bowel preparation quality. However, clinical significance seemed to be low. The presence of diverticula was an independent predictive factor for suboptimal bowel preparation quality.
Keyword
Figure
Cited by 2 articles
-
Author's Reply
Hoonsub So, Seungbong Han, Dong-Hoon Yang
Intest Res. 2015;13(4):364-364. doi: 10.5217/ir.2015.13.4.364.Letter: Patient Description of Rectal Effluents With Photographic Examples as a Predictive Indicator for the Quality of Bowel Preparation
Hyoun Woo Kang
Intest Res. 2015;13(4):362-363. doi: 10.5217/ir.2015.13.4.362.
Reference
-
1. van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006; 101:343–350. PMID: 16454841.
Article2. Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003; 58:76–79. PMID: 12838225.
Article3. Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005; 61:378–384. PMID: 15758907.
Article4. Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc. 2011; 73:1207–1214. PMID: 21481857.5. Rex DK, Imperiale TF, Latinovich DR, Bratcher LL. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol. 2002; 97:1696–1700. PMID: 12135020.
Article6. Fatima H, Johnson CS, Rex DK. Patients' description of rectal effluent and quality of bowel preparation at colonoscopy. Gastrointest Endosc. 2010; 71:1244–1252. PMID: 20362286.7. Harewood GC, Wright CA, Baron TH. Assessment of patients' perceptions of bowel preparation quality at colonoscopy. Am J Gastroenterol. 2004; 99:839–843. PMID: 15128347.
Article8. Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G. A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc. 2000; 52:346–352. PMID: 10968848.9. Ness RM, Manam R, Hoen H, Chalasani N. Predictors of inadequate bowel preparation for colonoscopy. Am J Gastroenterol. 2001; 96:1797–1802. PMID: 11419832.10. Serper M, Gawron AJ, Smith SG, et al. Patient factors that affect quality of colonoscopy preparation. Clin Gastroenterol Hepatol. 2014; 12:451–457. PMID: 23954647.11. Borg BB, Gupta NK, Zuckerman GR, Banerjee B, Gyawali CP. Impact of obesity on bowel preparation for colonoscopy. Clin Gastroenterol Hepatol. 2009; 7:670–675. PMID: 19245852.12. Sugihara K, Muto T, Morioka Y, Asano A, Yamamoto T. Diverticular disease of the colon in Japan. A review of 615 cases. Dis Colon Rectum. 1984; 27:531–537. PMID: 6468190.13. Kim SY, Oh TH, Seo JY, et al. The clinical factors for predicting severe diverticulitis in Korea: a comparison with Western countries. Gut Liver. 2012; 6:78–85. PMID: 22375175.14. Cooper GS, Xu F, Schluchter MD, Koroukian SM, Barnholtz Sloan JS. Diverticulosis and the risk of interval colorectal cancer. Dig Dis Sci. 2014; 59:2765–2772. PMID: 24927800.15. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology. 2007; 132:96–102. PMID: 17241863.16. Erichsen R, Baron JA, Stoffel EM, Laurberg S, Sandler RS, Sorensen HT. Characteristics and survival of interval and sporadic colorectal cancer patients: a nationwide population-based cohort study. Am J Gastroenterol. 2013; 108:1332–1340. PMID: 23774154.17. Kang MS, Kim TO, Seo EH, et al. Comparison of the efficacy and tolerability between same-day picosulfate and split-dose polyethylene glycol bowel preparation for afternoon colonoscopy: a prospective, randomized, investigator-blinded trial. Intest Res. 2014; 12:53–59. PMID: 25349564.18. Moon CM, Park DI, Choe YG, et al. Randomized trial of 2-L polyethylene glycol + ascorbic acid versus 4-L polyethylene glycol as bowel cleansing for colonoscopy in an optimal setting. J Gastroenterol Hepatol. 2014; 29:1223–1228. PMID: 24955451.19. Kim HG, Huh KC, Koo HS, et al. Sodium picosulfate with magnesium citrate (SPMC) plus laxative is a good alternative to conventional large volume polyethylene glycol in bowel preparation: a multicenter randomized single-blinded trial. Gut Liver. doi: 10.5009/gnl14010 Published online ahead of print 7 October 2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Description of Rectal Effluents With Photographic Examples as a Predictive Indicator for the Quality of Bowel Preparation
- Safe and appropriate use of laxatives for colonoscopy
- Bowel Preparation for Surveillance Colonoscopy After Colorectal Resection: A New Perspective
- A Review of Bowel Preparation Before Colorectal Surgery
- Comparison of Oral Sulfate Solution and Polyethylene Glycol Plus Ascorbic Acid on the Efficacy of Bowel Preparation