J Adv Prosthodont.
2013 May;5(2):179-186. 10.4047/jap.2013.5.2.179.
Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: two- and three-dimensional replica techniques
- Affiliations
-
- 1Department of Dental Laboratory Science and Engineering, Korea University, Seoul, Republic of Korea. kjh2804@korea.ac.kr
- KMID: 2284759
- DOI: http://doi.org/10.4047/jap.2013.5.2.179
Abstract
- PURPOSE
One of the most important factors in evaluating the quality of fixed dental prostheses (FDPs) is their gap. The purpose of this study was to compare the marginal and internal gap of two different metal-ceramic crowns, casting and selective laser sintering (SLS), before and after porcelain firing. Furthermore, this study evaluated whether metal-ceramic crowns made using the SLS have the same clinical acceptability as crowns made by the traditional casting.
MATERIALS AND METHODS
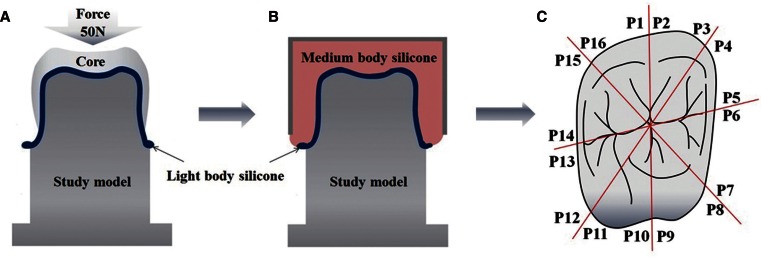
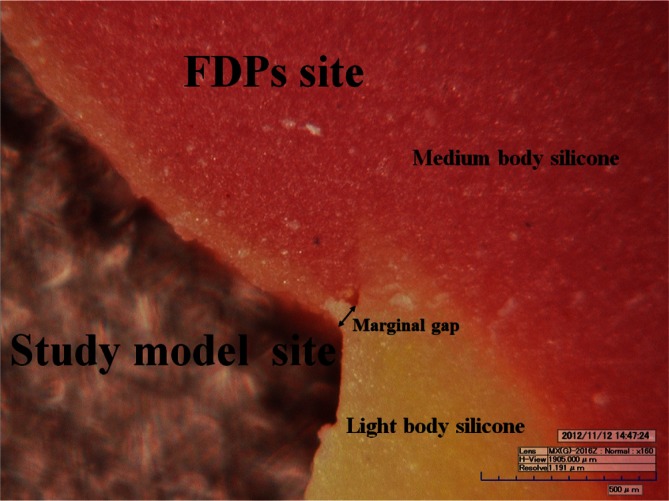
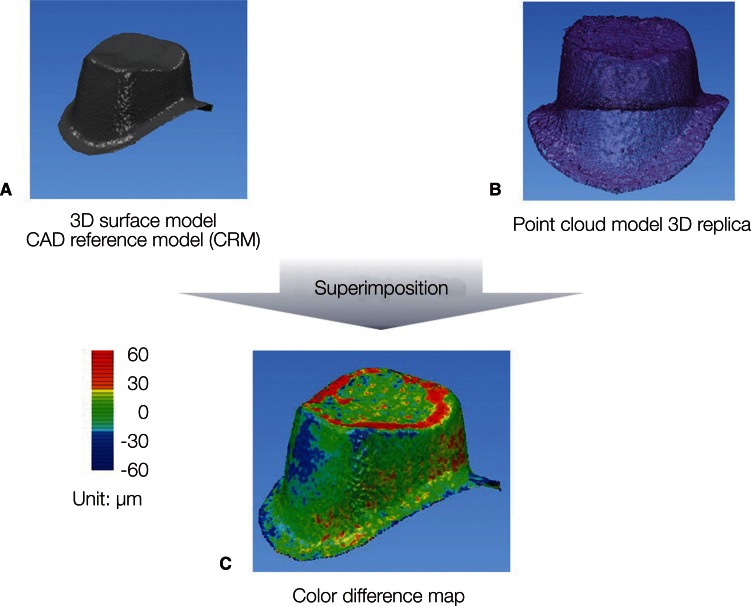
The 10 study models were produced using stone. The 20 specimens were produced using the casting and the SLS methods; 10 samples were made in each group. After the core gap measurements, 10 metal-ceramic crowns in each group were finished using the conventional technique of firing porcelain. The gap of the metal-ceramic crowns was measured. The marginal and internal gaps were measured by two-dimensional and three-dimensional replica techniques, respectively. The Wilcoxon signed-rank test, the Wilcoxon rank-sum test and nonparametric ANCOVA were used for statistical analysis (alpha=.05).
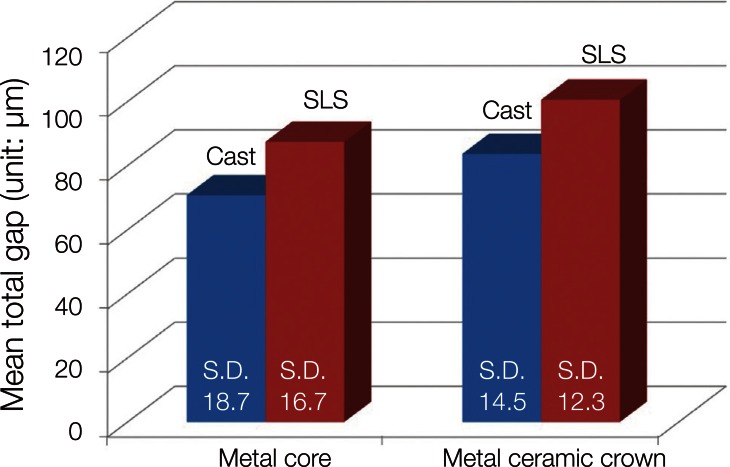
RESULTS
In both groups, the gap increased after completion of the metal-ceramic crown compared to the core. In all measured areas, the gap of the metal cores and metal-ceramic crowns produced by the SLS was greater than that of the metal cores and metal-ceramic crowns produced using the casting. Statistically significant differences were found between cast and SLS (metal cores and metal-ceramic crown).
CONCLUSION
Although the gap of the FDPs produced by the SLS was greater than that of the FDPs produced by the conventional casting in all measured areas, none exceeded the clinically acceptable range.
MeSH Terms
Figure
Cited by 2 articles
-
Influence of the accuracy of abutment tooth preparation on the marginal adaptation of Co-Cr alloy copings fabricated with a selective laser sintering technology
Seo-Rahng Kim, Jai-Young Koak, Seong-Joo Heo, Seong-Kyun Kim, Myung-Joo Kim
J Korean Acad Prosthodont. 2015;53(4):337-344. doi: 10.4047/jkap.2015.53.4.337.Marginal fit of three different nanocomposite inlays fabricated with computer-aided design/computer-aided manufacturing (CAD/CAM) technology: a comparative study
Hyunsuk Choi, Jae-Young Jo, Min-Ho Hong
J Yeungnam Med Sci. 2024;41(2):80-85. doi: 10.12701/jyms.2023.00934.
Reference
-
1. Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009; 28:44–56. PMID: 19280967.
Article2. Akova T, Ucar Y, Tukay A, Balkaya MC, Brantley WA. Comparison of the bond strength of laser-sintered and cast base metal dental alloys to porcelain. Dent Mater. 2008; 24:1400–1404. PMID: 18417202.
Article3. Campbell SD, Pelletier LB. Thermal cycling distortion of metal ceramics: Part I--Metal collar width. J Prosthet Dent. 1992; 67:603–608. PMID: 1527741.
Article4. Fonseca JC, Henriques GE, Sobrinho LC, de Góes MF. Stress-relieving and porcelain firing cycle influence on marginal fit of commercially pure titanium and titanium-aluminum-vanadium copings. Dent Mater. 2003; 19:686–691. PMID: 12901996.
Article5. Lakhani SA, Ercoli C, Moss ME, Graser GN, Tallents RH. Influence of cold working and thermal treatment on the fit of implant-supported metal-ceramic fixed partial dentures. J Prosthet Dent. 2002; 88:159–169. PMID: 12397243.
Article6. Pierce LH, Goodkind RJ. A status report of possible risks of base metal alloys and their components. J Prosthet Dent. 1989; 62:234–238. PMID: 2668518.
Article7. Wassell RW, Walls AW, Steele JG. materials selection. Br Dent J. 2002; 192:199–202. 205–211. PMID: 11931483.8. Vigolo P, Fonzi F. An in vitro evaluation of fit of zirconium-oxide-based ceramic four-unit fixed partial dentures, generated with three different CAD/CAM systems, before and after porcelain firing cycles and after glaze cycles. J Prosthodont. 2008; 17:621–626. PMID: 18798783.
Article9. Pak HS, Han JS, Lee JB, Kim SH, Yang JH. Influence of porcelain veneering on the marginal fit of Digident and Lava CAD/CAM zirconia ceramic crowns. J Adv Prosthodont. 2010; 2:33–38. PMID: 21165185.
Article10. Foster LV. Failed conventional bridge work from general dental practice: clinical aspects and treatment needs of 142 cases. Br Dent J. 1990; 168:199–201. PMID: 2180457.
Article11. Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater. 2009; 25:94–102. PMID: 18620749.
Article12. Kohorst P, Brinkmann H, Dittmer MP, Borchers L, Stiesch M. Influence of the veneering process on the marginal fit of zirconia fixed dental prostheses. J Oral Rehabil. 2010; 37:283–291. PMID: 20059649.
Article13. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns--validation of the silicone replica method. J Oral Rehabil. 2008; 35:116–122. PMID: 18197844.14. Groten M, Axmann D, Pröbster L, Weber H. Determination of the minimum number of marginal gap measurements required for practical in-vitro testing. J Prosthet Dent. 2000; 83:40–49. PMID: 10633021.15. Hung SH, Hung KS, Eick JD, Chappell RP. Marginal fit of porcelain-fused-to-metal and two types of ceramic crown. J Prosthet Dent. 1990; 63:26–31. PMID: 2404103.
Article16. Luthardt RG, Bornemann G, Lemelson S, Walter MH, Hüls A. An innovative method for evaluation of the 3-D internal fit of CAD/CAM crowns fabricated after direct optical versus indirect laser scan digitizing. Int J Prosthodont. 2004; 17:680–685. PMID: 15686096.17. Pelekanos S, Koumanou M, Koutayas SO, Zinelis S, Eliades G. Micro-CT evaluation of the marginal fit of different In-Ceram alumina copings. Eur J Esthet Dent. 2009; 4:278–292. PMID: 19704928.18. Ucar Y, Akova T, Akyil MS, Brantley WA. Internal fit evaluation of crowns prepared using a new dental crown fabrication technique: laser-sintered Co-Cr crowns. J Prosthet Dent. 2009; 102:253–259. PMID: 19782828.
Article19. Örtorp A, Jönsson D, Mouhsen A, Vult von Steyern P. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011; 27:356–363. PMID: 21163516.
Article20. Holmes JR, Bayne SC, Holland GA, Sulik WD. Considerations in measurement of marginal fit. J Prosthet Dent. 1989; 62:405–408. PMID: 2685240.
Article21. Bonate PL. Analysis of pretest-posttest designs. Boca Raton, FL: Chapman and Hall/CRC;2000. p. 98–100.22. White SN, Sorensen JA, Kang SK, Caputo AA. Microleakage of new crown and fixed partial denture luting agents. J Prosthet Dent. 1992; 67:156–161. PMID: 1538320.
Article23. Moldovan O, Luthardt RG, Corcodel N, Rudolph H. Three-dimensional fit of CAD/CAM-made zirconia copings. Dent Mater. 2011; 27:1273–1278. PMID: 21983002.
Article24. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns--validation of the silicone replica method. J Oral Rehabil. 2008; 35:116–122. PMID: 18197844.25. Rahme HY, Tehini GE, Adib SM, Ardo AS, Rifai KT. In vitro evaluation of the «replica technique» in the measurement of the fit of Procera crowns. J Contemp Dent Pract. 2008; 9:25–32. PMID: 18264522.26. Buchanan WT, Svare CW, Turner KA. The effect of repeated firings and strength on marginal distortion in two ceramometal systems. J Prosthet Dent. 1981; 45:502–506. PMID: 7012317.
Article27. Shokry TE, Attia M, Mosleh I, Elhosary M, Hamza T, Shen C. Effect of metal selection and porcelain firing on the marginal accuracy of titanium-based metal ceramic restorations. J Prosthet Dent. 2010; 103:45–52. PMID: 20105684.
Article28. Ostlund LE. Cavity design and mathematics: their effect on gaps at the margins of cast restorations. Oper Dent. 1985; 10:122–137. PMID: 3913900.29. Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont. 1997; 10:478–484. PMID: 9495168.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy evaluation of metal copings fabricated by computer-aided milling and direct metal laser sintering systems
- Comparative evaluation of marginal and internal fit of metal copings fabricated by various CAD/CAM methods
- Marginal and internal fit of all ceramic crown using the replica technique and the triple-scan protocol
- Marginal fit of the digident CAD/CAM zirconia ceramic crowns
- Fabricating a Ceramic-Pressed-to-Metal Restoration with Computer-Aided Design, Computer-Aided Manufacturing and Selective Laser Sintering: A Case Report