J Adv Prosthodont.
2014 Oct;6(5):387-394. 10.4047/jap.2014.6.5.387.
Surface treatment of feldspathic porcelain: scanning electron microscopy analysis
- Affiliations
-
- 1Department of Restorative Dentistry, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran. e.msalehi@yahoo.com
- KMID: 2284739
- DOI: http://doi.org/10.4047/jap.2014.6.5.387
Abstract
- PURPOSE
Topographic analysis of treated ceramics provides qualitative information regarding the surface texture affecting the micromechanical retention and locking of resin-ceramics. This study aims to compare the surface microstructure following different surface treatments of feldspathic porcelain.
MATERIALS AND METHODS
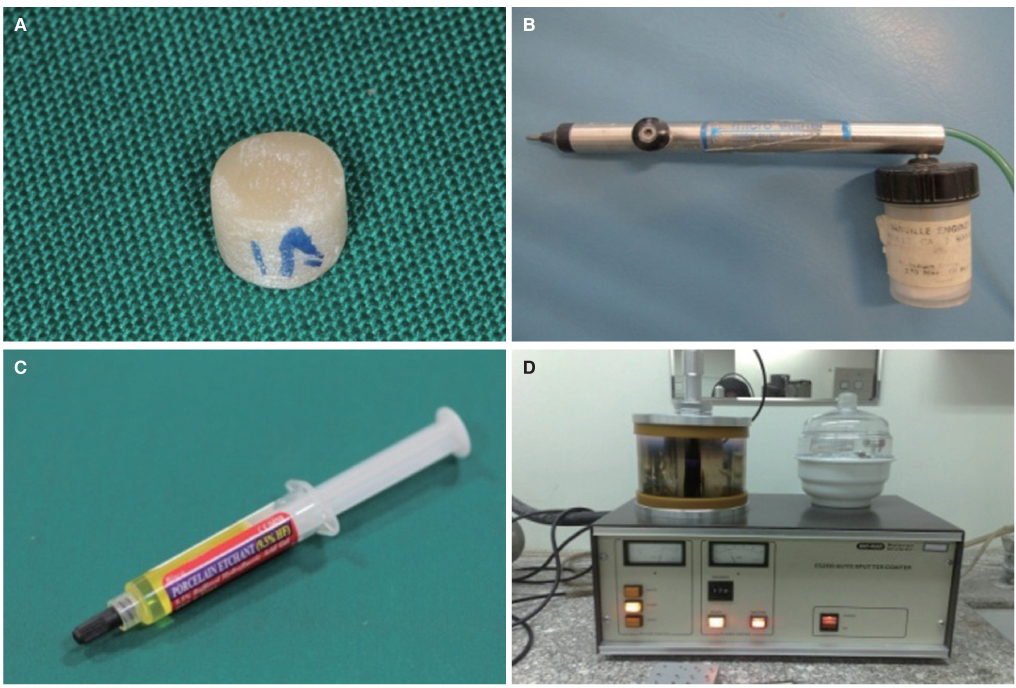
This in-vitro study was conducted on 72 porcelain discs randomly divided into 12 groups (n=6). In 9 groups, feldspathic surfaces were subjected to sandblasting at 2, 3 or 4 bar pressure for 5, 10 or 15 seconds with 50 microm alumina particles at a 5 mm distance. In group 10, 9.5% hydrofluoric acid (HF) gel was applied for 120 seconds. In group 11, specimens were sandblasted at 3 bar pressure for 10 seconds and then conditioned with HF. In group 12, specimens were first treated with HF and then sandblasted at 3 bar pressure for 10 seconds. All specimens were then evaluated under scanning electron microscopy (SEM) at different magnifications.
RESULTS
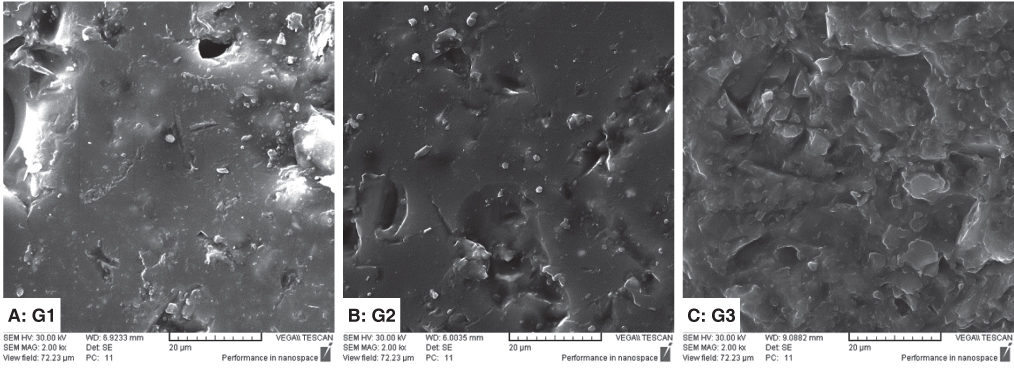
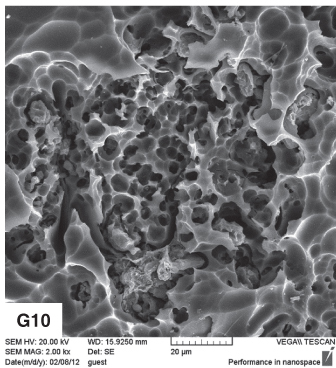
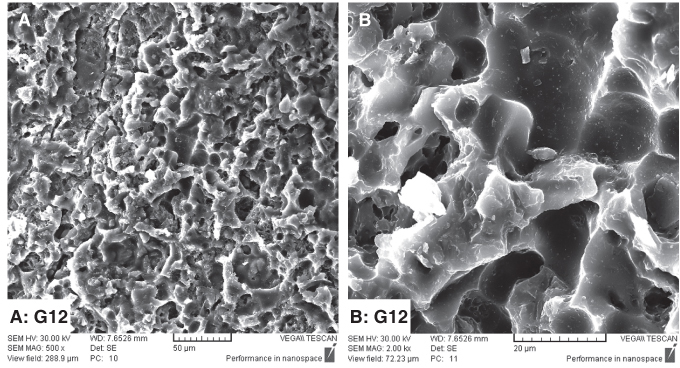
SEM images of HF treated specimens revealed deep porosities of variable sizes; whereas, the sandblasted surfaces were more homogenous and had sharper peaks. Increasing the pressure and duration of sandblasting increased the surface roughness. SEM images of the two combined techniques showed that in group 11 (sandblasted first), HF caused deeper porosities; whereas in group 12 (treated with HF first) sandblasting caused irregularities with less homogeneity.
CONCLUSION
All surface treatments increased the surface area and caused porous surfaces. In groups subjected to HF, the porosities were deeper than those in sandblasted only groups.
Keyword
MeSH Terms
Figure
Reference
-
1. Leinfelder KF. Dentin adhesives for the twenty-first century. Dent Clin North Am. 2001; 45:1–6.2. Kukiattrakoon B, Thammasitboon K. Optimal acidulated phosphate fluoride gel etching time for surface treatment of feldspathic porcelain: on shear bond strength to resin composite. Eur J Dent. 2012; 6:63–69.3. Gökçe B. Effects of Er: YAG laser irradiation on dental hard tissues and all-ceramic materials: SEM evaluation. 12 September, 2014. Available from: http://www.intechopen.com/books/scanning-electron-microscopy/effects-of-laser-irradiation-on-dental-hard-tissues-and-dental-materials-sem-evaluation-.4. Zarone F, Sorrentino R, Vaccaro F, Traini T, Russo S, Ferrari M. Acid etching surface treatment of feldspathic, alumina and zirconia ceramics: a micromorphological SEM analysis. Int Dent South Afr. 2006; 8:20–26.5. Torres SM, Borges GA, Spohr AM, Cury AA, Yadav S, Platt JA. The effect of surface treatments on the micro-shear bond strength of a resin luting agent and four all-ceramic systems. Oper Dent. 2009; 34:399–407.6. de Carvalho RF, Martins ME, de Queiroz JR, Leite FP, Ozcan M. Influence of silane heat treatment on bond strength of resin cement to a feldspathic ceramic. Dent Mater J. 2011; 30:392–397.7. Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003; 89:268–274.8. Kelly JR. Dental ceramics: what is this stuff anyway? J Am Dent Assoc. 2008; 139:4S–7S.9. Vargas MA, Bergeron C, Diaz-Arnold A. Cementing all-ceramic restorations: recommendations for success. J Am Dent Assoc. 2011; 142:20S–24S.10. de Melo RM, Valandro LF, Bottino MA. Microtensile bond strength of a repair composite to leucite-reinforced feldspathic ceramic. Braz Dent J. 2007; 18:314–319.11. El-Hosary MMK, Shokry TE, Zaki DY, El-Shakour ASA. Bond strength of different intraoral repair systems for metalceramic restorations. J Am Sci. 2011; 7:383–388.12. Reston EG, Filho SC, Arossi G, Cogo RB, Rocha Cdos S, Closs LQ. Repairing ceramic restorations: final solution or alternative procedure? Oper Dent. 2008; 33:461–466.13. Falkensammer F, Jonke E, Bertl M, Freudenthaler J, Bantleon HP. Rebonding performance of different ceramic brackets conditioned with a new silane coupling agent. Eur J Orthod. 2013; 35:103–109.14. Yadav S, Upadhyay M, Borges GA, Roberts WE. Influence of ceramic (feldspathic) surface treatments on the microshear bond strength of composite resin. Angle Orthod. 2010; 80:577–582.15. Ersu B, Yuzugullu B, Ruya Yazici A, Canay S. Surface roughness and bond strengths of glass-infiltrated alumina-ceramics prepared using various surface treatments. J Dent. 2009; 37:848–856.16. Osorio E, Toledano M, da Silveira BL, Osorio R. Effect of different surface treatments on In-Ceram Alumina roughness. An AFM study. J Dent. 2010; 38:118–122.17. Kupiec KA, Wuertz KM, Barkmeier WW, Wilwerding TM. Evaluation of porcelain surface treatments and agents for composite-to-porcelain repair. J Prosthet Dent. 1996; 76:119–124.18. Pollington S, Fabianelli A, van Noort R. Microtensile bond strength of a resin cement to a novel fluorcanasite glass-ceramic following different surface treatments. Dent Mater. 2010; 26:864–872.19. Barghi N, Fischer DE, Vatani L. Effects of porcelain leucite content, types of etchants, and etching time on porcelaincomposite bond. J Esthet Restor Dent. 2006; 18:47–52.20. Kara HB, Dilber E, Koc O, Ozturk AN, Bulbul M. Effect of different surface treatments on roughness of IPS Empress 2 ceramic. Lasers Med Sci. 2012; 27:267–272.21. Retief DH. Standardizing laboratory adhesion tests. Am J Dent. 1991; 4:231–236.22. Della Bona A, Donassollo TA, Demarco FF, Barrett AA, Mecholsky JJ Jr. Characterization and surface treatment effects on topography of a glass-infiltrated alumina/zirconia-reinforced ceramic. Dent Mater. 2007; 23:769–775.23. Darvell BW. Materials science for dentistry. 9th ed. UK: Elsevier;2009. p. 450–470.24. Amin Salehi E, Heshmat H, Moravej Salehi E, Kharazifard M. In vitro evaluation of the effect of different sandblasting times on the bond strength of feldspathic porcelain to composite resin. J Islam Dent Assoc IRAN. 2013; 25:22–30.25. Della Bona A, Anusavice KJ. Microstructure, composition, and etching topography of dental ceramics. Int J Prosthodont. 2002; 15:159–167.26. Subaşı MG, İnan Ö. Evaluation of the topographical surface changes and roughness of zirconia after different surface treatments. Lasers Med Sci. 2012; 27:735–742.27. Bottino MC, Ozcan M, Coelho PG, Valandro LF, Bressiani JC, Bressiani AH. Micro-morphological changes prior to adhesive bonding: high-alumina and glassy-matrix ceramics. Braz Oral Res. 2008; 22:158–163.28. Saraç YS, Elekdag-Turk S, Saraç D, Turk T. Surface conditioning methods and polishing techniques effect on surface roughness of a feldspar ceramic. Angle Orthod. 2007; 77:723–728.29. Borges GA, Sophr AM, de Goes MF, Sobrinho LC, Chan DC. Effect of etching and airborne particle abrasion on the microstructure of different dental ceramics. J Prosthet Dent. 2003; 89:479–488.30. Dilber E, Yavuz T, Kara HB, Ozturk AN. Comparison of the effects of surface treatments on roughness of two ceramic systems. Photomed Laser Surg. 2012; 30:308–314.31. Cal-Neto JP, Castro S, Moura PM, Ribeiro D, Miguel JA. Influence of enamel sandblasting prior to etching on shear bond strength of indirectly bonded lingual appliances. Angle Orthod. 2011; 81:149–152.32. Ozcan M. Evaluation of alternative intra-oral repair techniques for fractured ceramic-fused-to-metal restorations. J Oral Rehabil. 2003; 30:194–203.33. Kulunk S, Kulunk T, Ural C, Kurt M, Baba S. Effect of air abrasion particles on the bond strength of adhesive resin cement to zirconia core. Acta Odontol Scand. 2011; 69:88–94.34. Yavuz T, Dilber E, Kara HB, Tuncdemir AR, Ozturk AN. Effects of different surface treatments on shear bond strength in two different ceramic systems. Lasers Med Sci. 2013; 28:1233–1239.35. Schmage P, Nergiz I, Herrmann W, Ozcan M. Influence of various surface-conditioning methods on the bond strength of metal brackets to ceramic surfaces. Am J Orthod Dentofacial Orthop. 2003; 123:540–546.36. Wood DJ, Bubb NL, Millar BJ, Dunne SM. Preliminary investigation of a novel retentive system for hydrofluoric acid etch-resistant dental ceramics. J Prosthet Dent. 1997; 78:275–280.37. Torres SM, Borges GA, Spohr AM, Cury AA, Yadav S, Platt JA. The effect of surface treatments on the micro-shear bond strength of a resin luting agent and four all-ceramic systems. Oper Dent. 2009; 34:399–407.38. Saraç YŞ, Külünk T, Elekdağ-Türk S, Saraç D, Türk T. Effects of surface-conditioning methods on shear bond strength of brackets bonded to different all-ceramic materials. Eur J Orthod. 2011; 33:667–672.39. Lacy AM, LaLuz J, Watanabe LG, Dellinges M. Effect of porcelain surface treatment on the bond to composite. J Prosthet Dent. 1988; 60:288–291.40. Falkensammer F, Freudenthaler J, Pseiner B, Bantleon HP. Influence of surface conditioning on ceramic microstructure and bracket adhesion. Eur J Orthod. 2012; 34:498–504.41. Kern M, Barloi A, Yang B. Surface conditioning influences zirconia ceramic bonding. J Dent Res. 2009; 88:817–822.42. Herion DT, Ferracane JL, Covell DA Jr. Porcelain surface alterations and refinishing after use of two orthodontic bonding methods. Angle Orthod. 2010; 80:167–174.43. Türk T, Saraç D, Saraç YS, Elekdağ-Türk S. Effects of surface conditioning on bond strength of metal brackets to allceramic surfaces. Eur J Orthod. 2006; 28:450–456.44. Kara HB, Ozturk AN, Aykent F, Koc O, Ozturk B. The effect of different surface treatments on roughness and bond strength in low fusing ceramics. Lasers Med Sci. 2011; 26:599–604.45. Zogheib LV, Bona AD, Kimpara ET, McCabe JF. Effect of hydrofluoric acid etching duration on the roughness and flexural strength of a lithium disilicate-based glass ceramic. Braz Dent J. 2011; 22:45–50.46. Loomans BA, Mine A, Roeters FJ, Opdam NJ, De Munck J, Huysmans MC, Van Meerbeek B. Hydrofluoric acid on dentin should be avoided. Dent Mater. 2010; 26:643–649.47. Fabianelli A, Pollington S, Papacchini F, Goracci C, Cantoro A, Ferrari M, van Noort R. The effect of different surface treatments on bond strength between leucite reinforced feldspathic ceramic and composite resin. J Dent. 2010; 38:39–43.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A qualitative analysis of bonding between electroformed surface and veneering ceramics
- Shear bond strengths of composite resin to porcelains among porcelain repair systems
- An in-vitro wear study of human enamel opposing heat-pressed ceramics
- Metal-ceramic bond strength between a feldspathic porcelain and a Co-Cr alloy fabricated with Direct Metal Laser Sintering technique
- Spectrophotometric analysis of feldspathic porcelain with silver ion