J Adv Prosthodont.
2014 Dec;6(6):521-527. 10.4047/jap.2014.6.6.521.
Alveolar ridge preservation of an extraction socket using autogenous tooth bone graft material for implant site development: prospective case series
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Republic of Korea. kyk0505@snubh.org
- 2Department of Dentistry and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
- 3R&D Department, Korea Tooth Bank, Seoul, Republic of Korea.
- 4Department of Periodontology, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
- 5Department of Prosthodontics, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
- 6Department of Conservative Dentistry, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
- 7Department of Periodontology, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
- KMID: 2284727
- DOI: http://doi.org/10.4047/jap.2014.6.6.521
Abstract
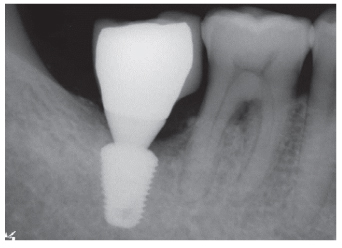
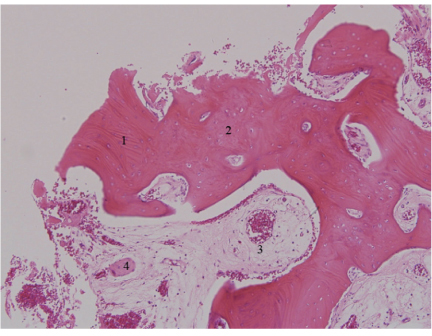
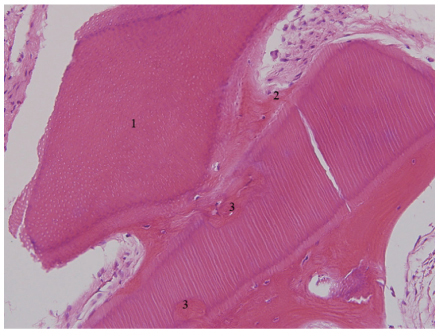
- This case series evaluated the clinical efficacy of autogenous tooth bone graft material (AutoBT) in alveolar ridge preservation of an extraction socket. Thirteen patients who received extraction socket graft using AutoBT followed by delayed implant placements from Nov. 2008 to Aug. 2010 were evaluated. A total of fifteen implants were placed. The primary and secondary stability of the placed implants were an average of 58 ISQ and 77.9 ISQ, respectively. The average amount of crestal bone loss around the implant was 0.05 mm during an average of 22.5 months (from 12 to 34 months) of functional loading. Newly formed tissues were evident from the 3-month specimen. Within the limitations of this case, autogenous tooth bone graft material can be a favorable bone substitute for extraction socket graft due to its good bone remodeling and osteoconductivity.
MeSH Terms
Figure
Reference
-
1. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32:212–218.2. Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, Orsini M. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997; 68:563–570.3. Camargo PM, Lekovic V, Weinlaender M, Klokkevold PR, Kenney EB, Dimitrijevic B, Nedic M, Jancovic S, Orsini M. Influence of bioactive glass on changes in alveolar process dimensions after exodontia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:581–586.4. Gross J. Ridge preservation using HTR synthetic bone following tooth extraction. Gen Dent. 1995; 43:364–367.5. Hämmerle CH, Chiantella GC, Karring T, Lang NP. The effect of a deproteinized bovine bone mineral on bone regeneration around titanium dental implants. Clin Oral Implants Res. 1998; 9:151–162.6. Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C, Bohra AA, Scheetz JP. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003; 74:990–999.7. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998; 69:1044–1049.8. Jeong KI, Kim SG, Kim YK, Oh JS, Jeong MA, Park JJ. Clinical study of graft materials using autogenous teeth in maxillary sinus augmentation. Implant Dent. 2011; 20:471–475.9. Jeong KI, Kim SG, Oh JS, Lim SC. Maxillary sinus augmentation using autogenous teeth: preliminary report. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:256–263.10. Kim YK, Lee HJ, Kim KW, Kim SG, Um IW. Guide bone regeneration using autogenous teeth: case reports. J Korean Assoc Oral Maxillofac Surg. 2011; 37:142–147.11. Darby I, Chen S, De Poi R. Ridge preservation: what is it and when should it be considered. Aust Dent J. 2008; 53:11–21.12. Luczyszyn SM, Papalexiou V, Novaes AB Jr, Grisi MF, Souza SL, Taba M Jr. Acellular dermal matrix and hydroxyapatite in prevention of ridge deformities after tooth extraction. Implant Dent. 2005; 14:176–184.13. Shi B, Zhou Y, Wang YN, Cheng XR. Alveolar ridge preservation prior to implant placement with surgical-grade calcium sulfate and platelet-rich plasma: a pilot study in a canine model. Int J Oral Maxillofac Implants. 2007; 22:656–665.14. Wang HL, Tsao YP. Histologic evaluation of socket augmentation with mineralized human allograft. Int J Periodontics Restorative Dent. 2008; 28:231–237.15. Artzi Z, Nemcovsky CE. The application of deproteinized bovine bone mineral for ridge preservation prior to implantation. Clinical and histological observations in a case report. J Periodontol. 1998; 69:1062–1067.16. Ten Heggeler JM, Slot DE, Van der Weijden GA. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res. 2011; 22:779–788.17. Kim YK, Yun PY, Lee HJ, Ahn JY, Kim SG. Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts. Implant Dent. 2011; 20:267–272.18. Lee HJ, Kim MJ, Kim YK, Yun PY. Extraction socket preservation using β-TCP coated with recombinant human BMP (rhBMP-2): randomized clinical prospective study. Oral Biol Res. 2011; 35:110–115.19. Jeong HR, Hwang JH, Lee JK. Effectiveness of autogenous tooth bone used as a graft material for regeneration of bone in miniature pig. J Korean Assoc Oral Maxillofac Surg. 2011; 37:375–379.20. Kim JY, Kim KW, Um IW, Kim YK, Lee JK. Bone healing capacity of demineralized dentin matrix materials in a minipig cranium defect. J Korean Dent Sci. 2012; 5:21–28.21. Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, Kim SY. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:496–503.22. Kim YK, Kim SG, Oh JS, Jin SC, Son JS, Kim SY, Lim SY. Analysis of the inorganic component of autogenous tooth bone graft material. J Nanosci Nanotech. 2011; 11:7442–7445.23. Murata M, Akazawa T, Hino J, Tazaki J, Ito K, Arisue M. Biochemical and histo-morphometrical analyses of bone and cartilage induced by human decalcified dentin matrix and BMP-2. Oral Biol Res. 2011; 35:9–14.24. Murata M, Sato D, Hino J, Akazawa T, Tazaki J, Ito K, Arisue M. Acid-insoluble human dentin as carrier material for recombinant human BMP-2. J Biomed Mater Res A. 2012; 100:571–577.25. Kim GW, Yeo IS, Kim SG, Um IW, Kim YK. Analysis of crystalline structure of autogenous tooth bone graft material: X-Ray diffraction analysis. J Korean Assoc Oral Maxillofac Surg. 2011; 37:225–228.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving oral rehabilitation through the preservation of the tissues through alveolar preservation
- Ridge Augmentation Using Block Type of Autogenous Tooth Bone Graft Material in Severe Alveolar Bone Resorption of Single Tooth: Case Report
- Autogenous fresh demineralized tooth graft prepared at chairside for dental implant
- Extraction Socket Preservation and Reconstruction Using Autogenous Tooth Bone Graft: Case Report
- Clinical Study on the Alveolar Bone Repair Capacity of Dentin Matrix Block