Healthc Inform Res.
2014 Jul;20(3):209-215. 10.4258/hir.2014.20.3.209.
Effectiveness and Sustainability of Education about Incident Reporting at a University Hospital in Japan
- Affiliations
-
- 1Department of Gastroenterological Surgery, Faculty of Medicine, Fukuoka University, Fukuoka, Japan. nn0904@fukuoka-u.ac.jp
- 2Department of Public Health & Preventive Medicine, Faculty of Medicine, Fukuoka University, Fukuoka, Japan.
- 3Department of Nursing, Fukuoka University Hospital, Fukuoka, Japan.
- KMID: 2284584
- DOI: http://doi.org/10.4258/hir.2014.20.3.209
Abstract
OBJECTIVES
The aim of this study was to evaluate the effectiveness and sustainability of educational interventions to encourage incident reporting.
METHODS
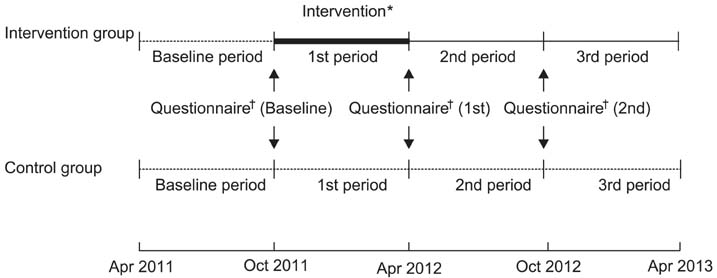
This was a quasi-experimental design. The study involved nurses working in two gastroenterology surgical wards at Fukuoka University Hospital, Japan. The number of participants on each ward was 26 nurses at baseline. For the intervention group, we provided 15 minutes of education about patient safety and the importance of incident reporting once per month for six months. After the completion of the intervention, we compared incident reporting in the subsequent 12 months for both groups. Questionnaires about reasons/motives for reporting were administered three times, before the intervention, after the intervention, and six months after the intervention for both the intervention group and the control group.
RESULTS
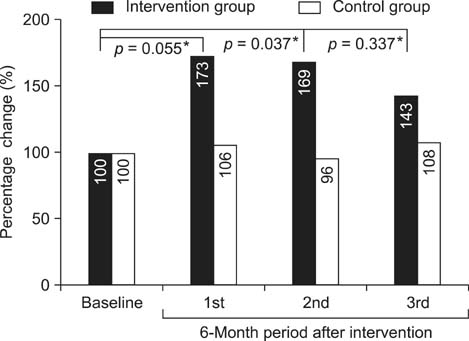
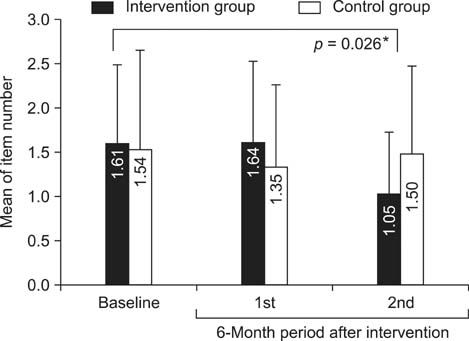
For the intervention group, incident reporting during the 6 months after the intervention period increased significantly compared with the baseline. During the same period, the reasons and motives for reporting changed significantly in the intervention group. The increase in reported incidents during the 6- to 12-month period following the intervention was not significant. In the control group, there was no significant difference during follow-up compared with the baseline.
CONCLUSIONS
A brief intervention about patient safety changed the motives for reporting incidents and the frequency of incidents reported by nurses working in surgical wards in a university hospital in Japan. However, the effect of the education decreased after six months following the education. Regular and long-term effort is required to maintain the effect of education.
Keyword
MeSH Terms
Figure
Reference
-
1. Leape LL. Error in medicine. JAMA. 1994; 272(23):1851–1857.
Article2. Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington (DC): National Academy Press;2000.3. Reason J. Human error: models and management. BMJ. 2000; 320(7237):768–770.
Article4. Vincent C, Taylor-Adams S, Chapman EJ, Hewett D, Prior S, Strange P, et al. How to investigate and analyse clinical incidents: clinical risk unit and association of litigation and risk management protocol. BMJ. 2000; 320(7237):777–781.
Article5. Naveh E, Katz-Navon T, Stern Z. Readiness to report medical treatment errors: the effects of safety procedures, safety information, and priority of safety. Med Care. 2006; 44(2):117–123.6. Hutchinson A, Young TA, Cooper KL, McIntosh A, Karnon JD, Scobie S, et al. Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and Learning System. Qual Saf Health Care. 2009; 18(1):5–10.
Article7. Mandavia R, Yassin G, Dhar V, Jacob T. Completing the audit cycle: the impact of an electronic reporting system on the feedback loop in surgical specialties. J Healthc Qual. 2013; 35(6):16–23.
Article8. Uribe CL, Schweikhart SB, Pathak DS, Dow M, Marsh GB. Perceived barriers to medical-error reporting: an exploratory investigation. J Healthc Manag. 2002; 47(4):263–279.
Article9. Evans SM, Smith BJ, Esterman A, Runciman WB, Maddern G, Stead K, et al. Evaluation of an intervention aimed at improving voluntary incident reporting in hospitals. Qual Saf Health Care. 2007; 16(3):169–175.
Article10. Sari AB, Sheldon TA, Cracknell A, Turnbull A. Sensitivity of routine system for reporting patient safety incidents in an NHS hospital: retrospective patient case note review. BMJ. 2007; 334(7584):79.
Article11. Christiaans-Dingelhoff I, Smits M, Zwaan L, Lubberding S, van der Wal G, Wagner C. To what extent are adverse events found in patient records reported by patients and healthcare professionals via complaints, claims and incident reports? BMC Health Serv Res. 2011; 11:49.
Article12. Hwang JI, Lee SI, Park HA. Barriers to the operation of patient safety incident reporting systems in Korean general hospitals. Healthc Inform Res. 2012; 18(4):279–286.
Article13. Welsh CH, Pedot R, Anderson RJ. Use of morning report to enhance adverse event detection. J Gen Intern Med. 1996; 11(8):454–460.
Article14. Evans SM, Berry JG, Smith BJ, Esterman A, Selim P, O'Shaughnessy J, et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care. 2006; 15(1):39–43.
Article15. Figueiras A, Herdeiro MT, Polonia J, Gestal-Otero JJ. An educational intervention to improve physician reporting of adverse drug reactions: a cluster-randomized controlled trial. JAMA. 2006; 296(9):1086–1093.
Article16. Jansma JD, Zwart DL, Leistikow IP, Kalkman CJ, Wagner C, Bijnen AB. Do specialty registrars change their attitudes, intentions and behaviour towards reporting incidents following a patient safety course? BMC Health Serv Res. 2010; 10:100.
Article17. Jansma JD, Wagner C, ten Kate RW, Bijnen AB. Effects on incident reporting after educating residents in patient safety: a controlled study. BMC Health Serv Res. 2011; 11:335.
Article18. Vincent C, Stanhope N, Crowley-Murphy M. Reasons for not reporting adverse incidents: an empirical study. J Eval Clin Pract. 1999; 5(1):13–21.
Article19. Russell J, Hollander S. A biology attitude scale. Am Biol Teach. 1975; 37(5):270–273.
Article20. Lovelace M, Brickman P. Best practices for measuring students' attitudes toward learning science. CBE Life Sci Educ. 2013; 12(4):606–617.
Article21. Barach P, Small SD. Reporting and preventing medical mishaps: lessons from non-medical near miss reporting systems. BMJ. 2000; 320(7237):759–763.
Article22. Firth-Cozens J. Barriers to incident reporting. Qual Saf Health Care. 2002; 11(1):7.
Article23. Coyle YM, Mercer SQ, Murphy-Cullen CL, Schneider GW, Hynan LS. Effectiveness of a graduate medical education program for improving medical event reporting attitude and behavior. Qual Saf Health Care. 2005; 14(5):383–388.
Article24. Kim J, Kim S, Jung Y, Kim EK. Status and problems of adverse event reporting systems in Korean hospitals. Healthc Inform Res. 2010; 16(3):166–176.
Article25. Yap J, Lee VJ, Yau TY, Ng TP, Tor PC. Knowledge, attitudes and practices towards pandemic influenza among cases, close contacts, and healthcare workers in tropical Singapore: a cross-sectional survey. BMC Public Health. 2010; 10:442.
Article26. Cronenwett L, Sherwood G, Barnsteiner J, Disch J, Johnson J, Mitchell P, et al. Quality and Safety Education for Nurses. Nurs Outlook. 2007; 55(3):122–131.
Article27. Tabali M, Jeschke E, Bockelbrink A, Witt CM, Willich SN, Ostermann T, et al. Educational intervention to improve physician reporting of adverse drug reactions (ADRs) in a primary care setting in complementary and alternative medicine. BMC Public Health. 2009; 9:274.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Nurses' Incident Reporting Attitude, Perception of Importance on Patient Safety Management, and Patient Safety Culture on the Reporting of Patient Safety Events
- Barriers to the Operation of Patient Safety Incident Reporting Systems in Korean General Hospitals
- Development of Electronic Incident Reporting System to Manage Medical Errors - Focused on Nursing Related Task
- Designing the Medical Education Program towards the Next Millennium in an Environment of the Higher Education Reform and Society Changes
- Effectiveness of a Mindfulness-Based Intervention in Older People Exposed to Trauma During the Jeju 4·3 Incident