Ewha Med J.
2013 Mar;36(1):43-50. 10.12771/emj.2013.36.1.43.
Does the Size of Anterior Microforaminotomy Affect the Surgical Outcome?
- Affiliations
-
- 1Department of Neurosurgery, Ewha Womans University School of Medicine, Seoul, Korea. kimmh@ewha.ac.kr
- KMID: 2284014
- DOI: http://doi.org/10.12771/emj.2013.36.1.43
Abstract
OBJECTIVES
Anterior microforaminotomy (AMF) is an alternative procedure to treat unilateral cervical pathology. Although the results have been reported favorable in the previous studies, postoperative degeneration may occur. We analyze long-term outcome to determine the critical size of AMF.
METHODS
A retrospective study was performed. Clinical data with chart review, radiologic data with picture archiving and communication system (PACS) images were obtained. Long-term clinical outcomes were accessed by a questionnaire, including visual analogue scale (VAS) and neck disability index (NDI). Various clinical, radiological data were statistically analyzed.
RESULTS
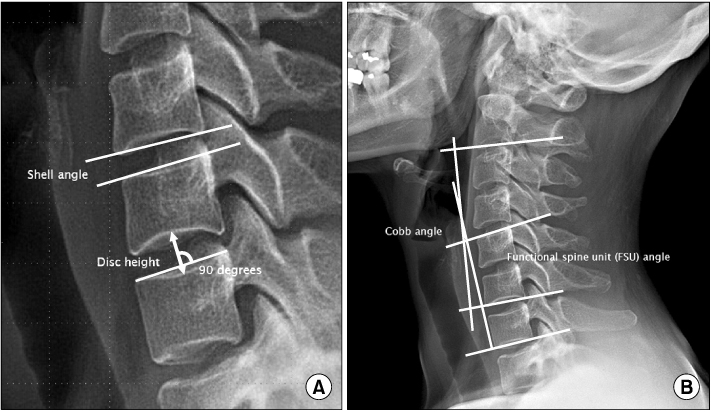
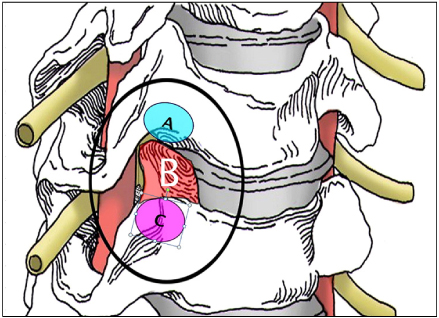
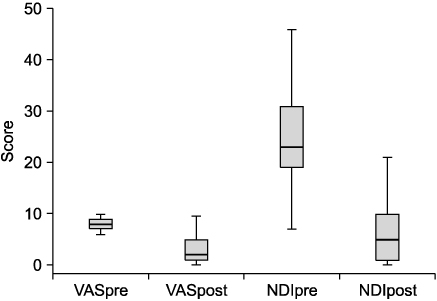
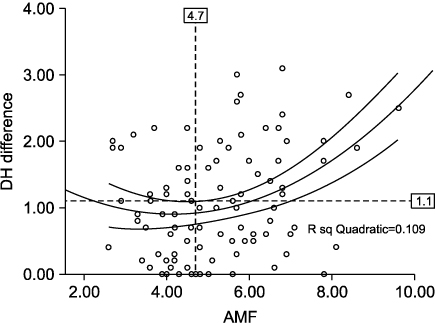
Eight-two patients were enrolled in this study. Main pathology was spondylotic spur (53.7%), soft disc herniation (36%). Mean age was 49 years old. There was no surgery-related complication. Mean follow-up was 6.1 years. 90.3% showed favorable clinical outcome. Mean VAS score was decreased from 8.2 to 2.9, and NDI score was decreased from 24.5 to 6.7 (P<0.05). 88.7% showed decrease of disc height (DH), and mean change was 1 mm. DH change was correlated positively with the disc invasion and AMF diameter (P<0.05). Mean diameter of AMF was 5.2 mm. According to statistical analysis, the critical diameter of AMF was 4.7 mm, directly affecting DH decrease. Any radiological parameters did not affect the clinical outcome.
CONCLUSION
AMF was an effective procedure to treat unilateral cervical pathology. Critical DH decreases and/or disc invasion may be the trigger of sequential degeneration. To preserve DH, AMF diameter should be small and disc invasion should be avoided.
Figure
Reference
-
1. Bertalanffy H, Eggert HR. Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy: a follow-up of 164 cases. Acta Neurochir (Wien). 1988. 90:127–135.2. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958. 15:602–617.3. Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, et al. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002. 51:840–847.4. Mosdal C. Cervical osteochondrosis and disc herniation. Eighteen years' use of interbody fusion by Cloward's technique in 755 cases. Acta Neurochir (Wien). 1984. 70:207–225.5. Murphey F, Simmons JC, Brunson B. Surgical treatment of laterally ruptured cervical disc: review of 648 cases, 1939 to 1972. J Neurosurg. 1973. 38:679–683.6. Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955. 96:223–224.7. Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993. 18:2167–2173.8. Elsawaf A, Mastronardi L, Roperto R, Bozzao A, Caroli M, Ferrante L. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurg Rev. 2009. 32:215–224.9. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999. 81:519–528.10. Hussain M, Natarajan RN, An HS, Andersson GB. Motion changes in adjacent segments due to moderate and severe degeneration in C5-C6 disc: a poroelastic C3-T1 finite element model study. Spine. 2010. 35:939–947.11. Nassr A, Lee JY, Bashir RS, Rihn JA, Eck JC, Kang JD, et al. Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine. 2009. 34:189–192.12. Pospiech J, Stolke D, Wilke HJ, Claes LE. Intradiscal pressure recordings in the cervical spine. Neurosurgery. 1999. 44:379–385.13. Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine. 2006. 31:2439–2448.14. Verbiest H. A lateral approach to the cervical spine: technique and indications. J Neurosurg. 1968. 28:191–203.15. Hakuba A. Trans-unco-discal approach. A combined anterior and lateral approach to cervical discs. J Neurosurg. 1976. 45:284–291.16. Snyder GM, Bernhardt M. Anterior cervical fractional interspace decompression for treatment of cervical radiculopathy: a review of the first 66 cases. Clin Orthop Relat Res. 1989. 246:92–99.17. Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg. 1996. 84:155–160.18. Balasubramanian C, Price R, Brydon H. Anterior cervical microforaminotomy for cervical radiculopathy--results and review. Minim Invasive Neurosurg. 2008. 51:258–262.19. Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J. 2007. 16:1387–1393.20. Cornelius JF, Bruneau M, George B. Microsurgical cervical nerve root decompression via an anterolateral approach: clinical outcome of patients treated for spondylotic radiculopathy. Neurosurgery. 2007. 61:972–980.21. Hong WJ, Kim WK, Park CW, Lee SG, Yoo CJ, Kim YB, et al. Comparison between transuncal approach and upper vertebral transcorporeal approach for unilateral cervical radiculopathy - a preliminary report. Minim Invasive Neurosurg. 2006. 49:296–301.22. Jho HD, Kim WK, Kim MH. Anterior microforaminotomy for treatment of cervical radiculopathy: part 1--disc-preserving "functional cervical disc surgery". Neurosurgery. 2002. 51:5 Suppl. S46–S53.23. Johnson JP, Filler AG, McBride DQ, Batzdorf U. Anterior cervical foraminotomy for unilateral radicular disease. Spine. 2000. 25:905–909.24. Kotil K, Bilge T. Prospective study of anterior cervical microforaminotomy for cervical radiculopathy. J Clin Neurosci. 2008. 15:749–756.25. Lee JY, Lohr M, Impekoven P, Koebke J, Ernestus RI, Ebel H, et al. Small keyhole transuncal foraminotomy for unilateral cervical radiculopathy. Acta Neurochir (Wien). 2006. 148:951–958.26. Saringer W, Nöbauer I, Reddy M, Tschabitscher M, Horaczek A. Microsurgical anterior cervical foraminotomy (uncoforaminotomy) for unilateral radiculopathy: clinical results of a new technique. Acta Neurochir (Wien). 2002. 144:685–694.27. White BD, Buxton N, Fitzgerald JJ. Anterior cervical foramenotomy for cervical radiculopathy. Br J Neurosurg. 2007. 21:370–374.28. Jho HD. Failed anterior cervical foraminotomy. J Neurosurg. 2003. 98:2 Suppl. 121–125.29. Hacker RJ, Miller CG. Failed anterior cervical foraminotomy. J Neurosurg. 2003. 98:2 Suppl. 126–130.30. Kotani Y, McNulty PS, Abumi K, Cunningham BW, Kaneda K, McAfee PC. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study. Spine. 1998. 23:1559–1565.31. Chen TY, Crawford NR, Sonntag VK, Dickman CA. Biomechanical effects of progressive anterior cervical decompression. Spine. 2001. 26:6–14.32. Okada E, Matsumoto M, Ichihara D, Chiba K, Toyama Y, Fujiwara H, et al. Aging of the cervical spine in healthy volunteers: a 10-year longitudinal magnetic resonance imaging study. Spine. 2009. 34:706–712.33. Walraevens J, Liu B, Meersschaert J, Demaerel P, Delye H, Depreitere B, et al. Qualitative and quantitative assessment of degeneration of cervical intervertebral discs and facet joints. Eur Spine J. 2009. 18:358–369.34. Osti OL, Vernon-Roberts B, Fraser RD. Anulus tears and intervertebral disc degeneration: an experimental study using an animal model. Spine. 1990. 15:762–767.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Cervical Microforaminotomy
- The Outcome of Anterior Microforaminotomy for Single Level Cervical Radicular Disease
- The Result of Posterior Microforaminotomy for Posterolateral Herniation of Cervical Discs
- Extent of Disc Degeneration after Single-Level Cervical Anterior Microforaminotomy Analyzed with Long-Term Radiological Data
- Morphometric Measurement of the Anatomical Landmark in Anterior Cervical Microforaminotomy