Korean J Perinatol.
2015 Sep;26(3):222-228. 10.14734/kjp.2015.26.3.222.
Clinical Manifestations of Capillary Hemangiomas in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea. revival421@empas.com
- 2Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
- KMID: 2281226
- DOI: http://doi.org/10.14734/kjp.2015.26.3.222
Abstract
- PURPOSE
Capillary hemangiomas occur more frequently in preterm infants. We aimed to describe the clinical course of capillary hemangiomas in preterm infants.
METHODS
The records of preterm infants with a gestational age (GA) of <35 weeks who were admitted to two tertiary neonatal intensive care units from January 2004 to December 2013 and had capillary hemangiomas were reviewed retrospectively. Subgroup analysis of between infants of GA <30 weeks and GA 30-34+6 weeks were done and ad hoc analysis comparing study population and matched preterm infants without hemangioma for investigation of differences in clinical characteristics.
RESULTS
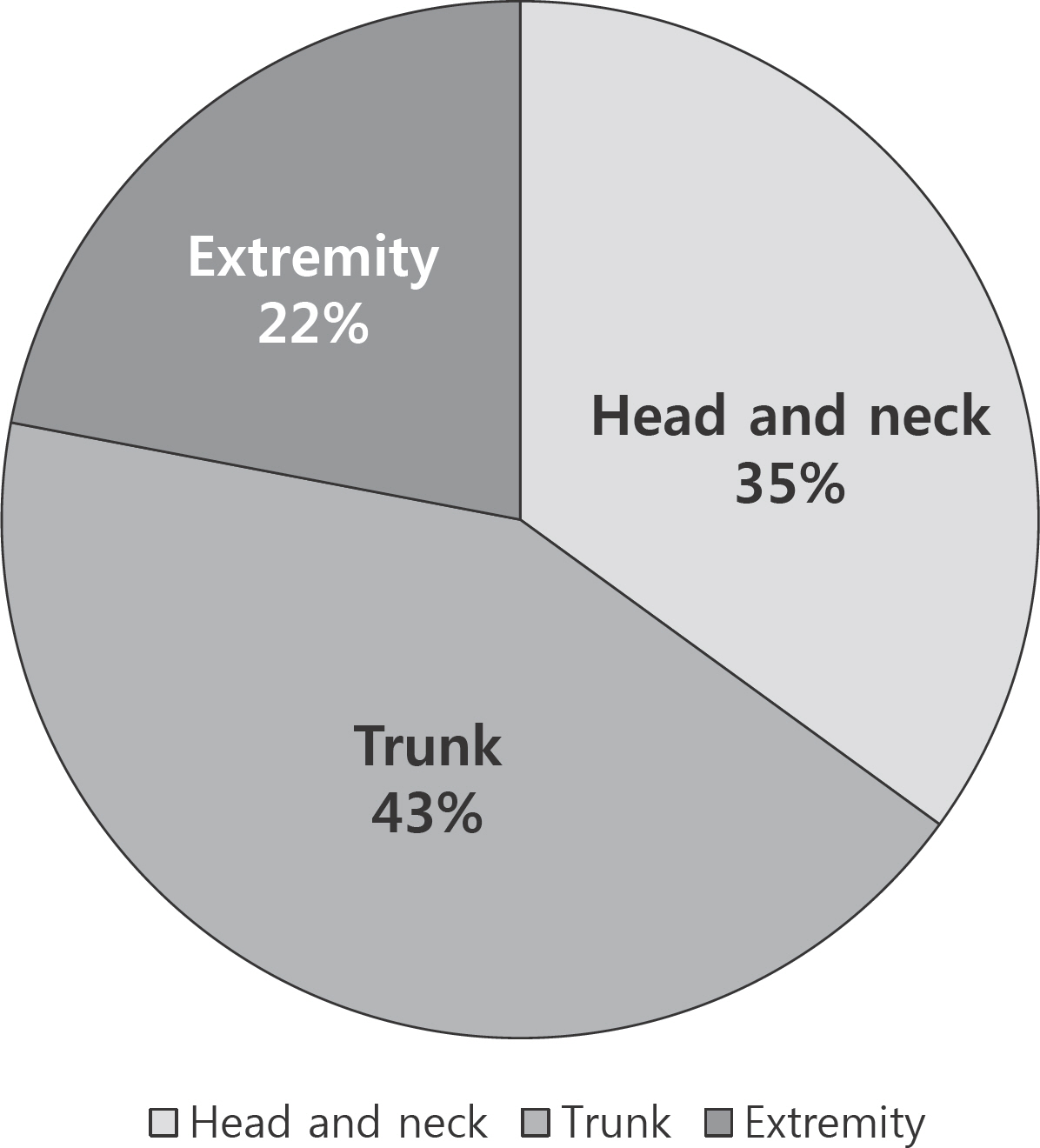
Of the 2,772 preterm infants, 112 (4%) infants developed capillary hemangiomas. The majority (91.9 %) of them had a solitary hemangiomas with the trunk was the most commonly involved site (43%). Three quarters of the patients were treated with topical corticosteroid, propranolol or laser treatment. When we divided this population as who were born before or after GA 30 weeks, there was no difference at postmenstrual age (PMA) of onset of capillary hemangiomas (median [IQR], 36(+4) [30(+5)-40(+5)] vs. 36+2 [33(+6)-41(+1)] weeks, P = 0.275). The age at involution of capillary hemangiomas was also not differ between two groups (median [IQR], 7.75 [3.75-12.25] vs. 7.5 [4-13.75] months, P=0.425). There were no statistical differences between preterm infants with capillary hemangiomas and their age, weight and sex matched control preterm infants without hemangiomas in the neonatal and maternal factors.
CONCLUSION
The development of capillary hemangiomas occurred at approximately 36 to 37 weeks of PMA regardless of prematurity in preterm infants. Capillary hemangiomas of preterm infants resolved spontaneously and disappear completely by around 7 months of corrected age.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Robb RM. Refractive errors associated with hemangiomas of the eyelids and orbit in infancy. Am J Ophthalmol. 1977; 83:52–8.
Article2. Stigmar G, Crawford JS, Ward CM, Thomson HG. Ophthalmic sequelae of infantile hemangiomas of the eyelids and orbit. Am J Ophthalmol. 1978; 85:806–13.
Article3. Haik BG, Jakobiec FA, Ellsworth RM, Jones IS. Capillary hemangioma of the lids and orbit: an analysis of the clinical features and therapeutic results in 101 cases. Ophthalmol. 1979; 86:760–92.
Article4. Drolet BA, Esterly NB, Frieden IJ. Hemangiomas in children. N Engl J Med. 1999; 341:173–81.
Article5. Orlow SJ, Isakoff MS, Blei F. Increased risk of symptomatic hemangiomas of the airway in association with cutaneous hemangiomas in a "beard" distribution. J Pediatr. 1997; 131:643–6.
Article6. Jacobs AH. Strawberry hemangiomas; the natural history of the untreated lesion. Calif Med. 1957; 86:8–10.
Article7. Hoornweg MJ, Smeulders MJ, Ubbink DT, van der Horst CM. The prevalence and risk factors of infantile haemangiomas: a case-control study in the Dutch population. Paediatr Perinat Epidemiol. 2012; 26:156–62.
Article8. Hidano A, Purwoko R, Jitsukawa K. Statistical survey of skin changes in Japanese neonates. Pediatr Dermatol. 1986; 3:140–4.
Article9. Shih IH, Lin JY, Chen CH, Hong HS. A birthmark survey in 500 newborns: clinical observation in two northern Taiwan medical center nurseries. Chang Gung Med J. 2007; 30:220–5.10. Drolet BA, Swanson EA, Frieden IJ. Infantile hemangiomas: an emerging health issue linked to an increased rate of low birth weight infants. J Pediatr. 2008; 153:712–5. 15 e1.
Article11. Chiller KG, Passaro D, Frieden IJ. Hemangiomas of infancy: clinical characteristics, morphologic subtypes, and their relationship to race, ethnicity, and sex. Arch Dermatol. 2002; 138:1567–76.12. Hyland RM, Komlosi K, Alleman BW, Tolnai M, Wood LM, Bell EF, et al. Infantile hemangiomas and retinopathy of prematurity: clues to the regulation of vasculogenesis. Eur J Pediatr. 2013; 172:803–9.
Article13. Amir J, Metzker A, Krikler R, Reisner SH. Strawberry hemangioma in preterm infants. Pediatr Dermatol. 1986; 3:331–2.
Article14. Praveen V, Vidavalur R, Rosenkrantz TS, Hussain N. Infantile hemangiomas and retinopathy of prematurity: possible association. Pediatrics. 2009; 123:e484–9.
Article15. Kim JS, Kim SY, Lee JY, Kim JH, Kim EK, Kim HS, et al. Optimal timing of the first screening examination for retinopathy of prematurity. Neonatal Med. 2013; 20:454–61.
Article16. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–9.
Article17. Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986; 33:179–201.
Article18. Ji Y, Chen S, Li K, Li L, Xu C, Xiang B. Signaling pathways in the development of infantile hemangioma. J Hematol Oncol. 2014; 7:13.
Article19. Pascual-Castroviejo I, Viano J, Moreno F, Palencia R, Martinez Fernandez V, Pascual-Pascual SI, et al. Hemangiomas of the head, neck, and chest with associated vascular and brain anomalies: a complex neurocutaneous syndrome. Am J Neuroradiol. 1996; 17:461–71.20. Kishnani P, Iafolla AK, McConkie-Rosell A, Van Hove JL, Kanter RJ, Kahler SG. Hemangioma, supraumbilical midline raphe, and coarctation of the aorta with a right aortic arch: single causal entity? Am J Med Genet. 1995; 59:44–8.21. Burton BK, Schulz CJ, Angle B, Burd LI. An increased incidence of haemangiomas in infants born following chorionic villus sampling (CVS). Prenat Diagn. 1995; 15:209–14.
Article22. Finn MC, Glowacki J, Mulliken JB. Congenital vascular lesions: clinical application of a new classification. J Pediatr Surg. 1983; 18:894–900.23. Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg. 2000; 37:517–84.
Article24. Sidoroff A. Epidemiology of cutaneous vascular neoplasms and malformations in childhood. Handchir Mikrochir Plast Chir. 2009; 41:65–9.25. Maguiness SM, Frieden IJ. Current management of infantile hemangiomas. Semin Cutan Med Surg. 2010; 29:106–14.
Article26. Leaute-Labreze C, Dumas de la Roque E, Hubiche T, Bora-levi F, Thambo JB, Taieb A. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008; 358:2649–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subcutaneous Cavernous and Capillary Hemangiomas of the Breast: Radiologic-Pathological Correlation
- Neurodevelopmental outcomes of preterm infants
- Clinical Characteristics of Apnea in Full-Term Infants: Compared to Late Preterm Infants
- Capillary Hemangioma of the Testis
- A Case of Capillary Hemangioma in the Jejunum Detected by Single Balloon Enteroscopy in a Patient with Anemia