Korean J Pediatr Infect Dis.
2013 Dec;20(3):190-196.
A Case of Tuberculous Enteritis with Active Pulmonary Tuberculosis in a 12-Year-Old Girl
- Affiliations
-
- 1Department of Pediatrics, Soonchunhyang University College of Medicine, Bucheon, Kyonggido, Korea. jop50@schmc.ac.kr
- 2Department of Pathology, Soonchunhyang University College of Medicine, Bucheon, Kyonggido, Korea.
Abstract
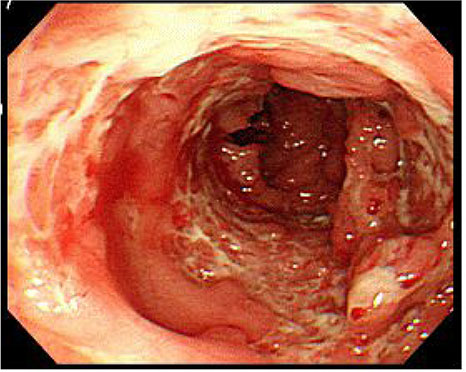
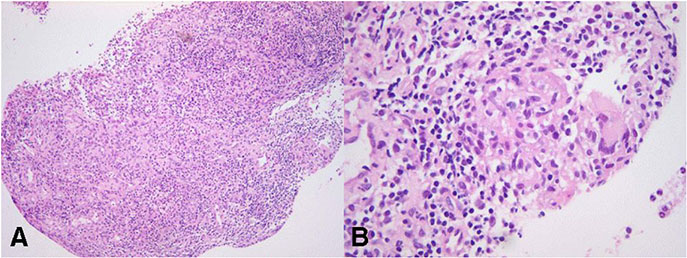
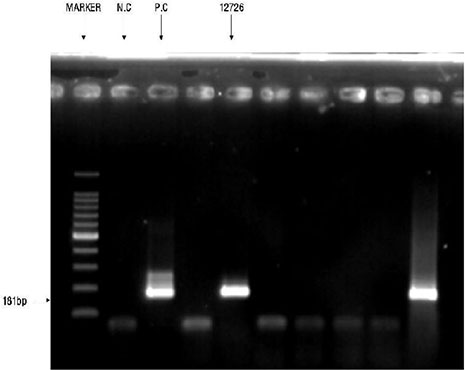
- Intestinal tuberculosis (TB) is presented with nonspecific and variable clinical manifestations such as abdominal pain, diarrhea, fever and weight loss. Diagnosis of tuberculous enteritis may be missed or confused with many other chronic gastrointestinal disorders such as the Crohn disease and intestinal neoplasms. The diagnosis should be based on careful clinical evaluations, such as extra-intestinal signs and colonoscopic and histologic findings. Newer techniques such as PCR tests from the specimens through colonoscopic biopsy may be helpful to confirm diagnosis of tuberculous enteritis. The treatment regimens for pulmonary tuberculosis are generally effective for tuberculous enteritis as well. If not treated early, the prognosis of intestinal tuberculosis is poor. We report a case of tuberculous enteritis diagnosed by colonoscopic biopsy and TB PCR which was presented with diarrhea, abdominal pain, intermittent fever and weight loss in a 12-year-old girl with active pulmonary tuberculosis. The patient was treated successfully with antituberculosis agents for 11 months without any complications.
MeSH Terms
Figure
Reference
-
1. Cho JY, Kim YS, Park WW, Chuan TP, Kim HT, Lee SR, et al. Clinical features of intestinal tuberculosis in recent ten years (2001-2010). Intest Res. 2011; 9:12–18.
Article2. Choi KM, Kim NH, Kim DH, Kim YJ, Kim JH, Oh SH, et al. Korean guidelines for diagnosis and treatment of tuberculosis in children and adolescents. Korean J Pediatr Infect Dis. 2011; 18:1–14.
Article3. Eun BW. Characteristics of tuberculosis in children and adolescents. Korean J Pediatr. 2009; 52:513–518.
Article4. Hwang KE, Jang NS, Park CY, Lim SY, Kim BI, Jeon WK, et al. Significance of colonoscopy in the early diagnosis of intestinal tuberculosis. Korean J Gastroenterol. 1997; 29:449–456.5. Kim SJ, Park SE, Lee MG, Kim GI, Lee CH, Park JH. A case of intestinal tuberculosis concurring with endobronchial and laryngeal tuberculosis. J Korean Pediatr Soc. 2003; 46:714–717.6. Bhargava DK. Abdominal tuberculosis: current status. Apollo Medicine. 2007; 4:287–291.
Article7. Yang SH, Chu MA, Park HJ, Lee KH, Kim JK, Choi EJ, et al. Clinical characteristics of tuberculosis in school-age children and adolescents at a single institution. Pediatr Allergy Respir Dis. 2012; 22:239–247.
Article8. Andronikou S, Welman CJ, Kader E. The CT features of abdominal tuberculosis in children. Pediatr Radiol. 2002; 32:75–81.
Article9. Choi SM, Yang SK, Jung HY, Ha HK, Yu CS, Kim JC, et al. Clinical features of intestinal tuberculosis with special reference to risk factors for complications. Korean J Gastroenterol. 1997; 30:462–471.10. Kim KM, Lee A, Choi KY, Lee KY, Kwak JJ. Intestinal tuberculosis: clinicopathologic analysis and diagnosis by endoscopic biopsy. Am J Gastroenterol. 1998; 93:606–609.
Article11. Lee YJ, Yang SK, Myung SJ, Byeon JS, Park IG, Kim JS, et al. The usefulness of colonoscopic biopsy in the diagnosis of intestinal tuberculosis and pattern of concomitant extra-intestinal tuberculosis. Korean J Gastroenterol. 2004; 44:153–159.12. Mitchell RS, Bristol LJ. Intestinal tuberculosis: an analysis of 346 cases diagnosed by routine intestinal radiography on 5,529 admissions for pulmonary tuberculosis, 1924-49. Am J Med Sci. 1954; 227:241–249.13. Oto BT, Fauzi A, Syam AF, Simadibrata M, Abdullah M, Makmun D, et al. Colitis tuberculosis. Indonesian J Gastroenterol Hepatol Dig Endosc. 2010; 11:143–149.14. Kim YS, Kim YH, Lee KM, Kim JS, Park YS. IBD Study Group of the Korean Association of the Study of Intestinal Diseases. Diagnostic guideline of intestinal tuberculosis. Korean J Gastroenterol. 2009; 53:177–186.15. Naval GR, Chua ML. Diagnosis of intestinal tuberculosis among patients with chronic diarrhea: role of intubation biopsy. Phil J Microbiol Infect Dis. 1998; 27:23–27.16. Lee YJ, Yang SK, Byeon JS, Myung SJ, Chang HS, Hong SS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006; 38:592–597.
Article17. Park SH, Yang SK, Yang DH, Kim KJ, Yoon SM, Choe JW, et al. Prospective randomized trial of six-month versus nine-month therapy for intestinal tuberculosis. Antimicrob Agents Chemother. 2009; 53:4167–4171.
Article18. Maroushek SR, Starke JR. Mycobacterial infections. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Saunders;2011. p. 996–1011.19. Youn JE, Park IB, Kwon SY, Kim JS, Byun KS, Park YT, et al. Follow-up colonoscopy at 3 months of therapy in patients with tentative diagnosis of intestinal tuberculosis. Korean J Med. 1996; 50:227–233.20. Ozbey H, Tireli GA, Salman T. Abdominal tuberculosis in children. Eur J Pediatr Surg. 2003; 13:116–119.
Article