Clin Exp Otorhinolaryngol.
2009 Sep;2(3):141-144.
The Surgical Outcome of Endoscopic Dacryocystorhinostomy According to the Obstruction Levels of Lacrimal Drainage System
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck surgery, Chungbuk National University, Cheongju, Korea. hwatas@dreamwiz.com
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Boramae Hospital, Seoul, Korea.
- 3Department of Ophthalmology, Chungbuk National University, Cheongju, Korea.
Abstract
OBJECTIVES
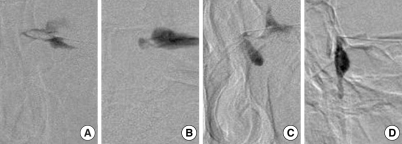
Many factors influence the outcome of endoscopic dacryocystorhinostomy (DCR). One of the most important prognostic factors is the level of obstruction in the lacrimal drainage system. The main objective of this report is to evaluate both the frequency of obstruction by anatomical region of the lacrimal drainage system on dacryocystography (DCG) and the surgical outcome of endoscopic DCR according to the obstruction level. METHODS: A retrospective series of 48 patients (60 eyes) who had undergone endoscopic DCR from January 2005 to November 2007 were enrolled. Preoperative evaluation consisted of a standard examination which included lacrimal irrigation, probing, DCG and osteomeatal unit (OMU) computed tomography. Patients were classified into four groups according to the obstruction level on DCG. Surgical outcome was evaluated postoperatively by subjective improvement of epiphora and patent rhinostomy opening on nasal endoscopic exam. RESULTS: Of 60 eyes, the levels of obstruction were the common canaliculus in 14 eyes (23.3%), the lacrimal sac in 13 eyes (21.7%), the duct-sac junction in 13 eyes (21.7%) and the nasolacrimal duct (NLD) in 20 eyes (33.3%). The ductsac junction obstruction was treated most successfully (100%), followed by NLD obstruction (90%), common canaliculus obstruction (78.6%) and saccal obstruction (69.2%). CONCLUSION: In patients with lacrimal drainage system obstruction, preoperative evaluation of obstruction level using DCG may be helpful for predicting the surgical outcome of endoscopic DCR. The saccal obstruction may have a worse prognosis than the other obstruction levels.
MeSH Terms
Figure
Reference
-
1. Song HY, Jin YH, Kim JH, Suh SW, Yoon HK, Kang SG, et al. Non-surgical placement of a nasolacrimal polyurethane stent: long-term effectiveness. Radiology. 1996; 9. 200(3):759–763. PMID: 8756928.
Article2. McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989; 6. 103(6):585–587. PMID: 2769026.
Article3. Watkins LM, Janfaza P, Rubin PA. The evolution of endonasal dacryocystorhinostomy. Surv Ophthalmol. 2003; Jan–Feb. 48(1):73–84. PMID: 12559328.
Article4. Metson R, Woog JJ, Puliafito CA. Endoscopic laser dacryocystorhinostomy. Laryngoscope. 1994; 3. 104(3 Pt 1):269–274. PMID: 8127181.
Article5. Hehar SS, Jones NS, Sadiq SA, Downes RN. Endoscopic holmium: YAG laser dacryocystorhinostomy-safe and effective as a day-case procedure. J Laryngol Otol. 1997; 11. 111(11):1056–1059. PMID: 9472576.
Article6. Sprekelsen MB, Barberan MT. Endoscopic dacryocystorhinostomy: surgical technique and results. Laryngoscope. 1996; 2. 106(2 Pt 1):187–189. PMID: 8583851.7. Weidenbecher M, Hosemann W, Buhr W. Endoscopic endonasal dacryocystorhinostomy: results in 56 patients. Ann Otol Rhinol Laryngol. 1994; 5. 103(5 Pt 1):363–367. PMID: 8179252.
Article8. Yung MW, Hardman-Lea S. Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol. 2002; 7. 86(7):792–794. PMID: 12084752.
Article9. Beigi B, Westlake W, Chang B, Marsh C, Jacob J, Chatfield J. Dacryocystorhinostomy in south west England. Eye. 1998; 12(Pt 3a):358–362. PMID: 9775231.
Article10. Hurwitz JJ, Rutherford S. Computerized survey of lacrimal surgery patients. Ophthalmology. 1986; 1. 93(1):14–19. PMID: 3951812.
Article11. McDonogh M. Endoscopic transnasal dacryocystorhinostomy: results in 21 patients. S Afr J Surg. 1992; 9. 30(3):107–110. PMID: 1411802.12. Kim JS, Ahn M. Clinical evaluation and classification of nasolacrimal duct obstruction site by dacryocystography. J Korean Ophthalmol Soc. 2005; 2. 46(2):191–195.13. Grover AK, Gupta AK, Rastogi A. Modified canaliculo-dacryocystorhinostomy. Indian J Ophthalmol. 1991; 10. 39(4):159–161. PMID: 1810875.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Definition and treatment of lacrimal drainage disease
- Surgical Outcomes of Dacryocystorhinostomy in Lacrimal Drainage Obstruction after Systemic Chemotherapy or Radioactive Iodine Therapy
- Endoscopic Dacryocystorhinostomy for the Treatment of Lacrimal Sac Abscess
- Results with Silicone Stent in Lacrimal Drainage System
- A Huge Dacryolith Presenting as a Mass of the Inferior Meatus