Clin Exp Otorhinolaryngol.
2014 Jun;7(2):153-156.
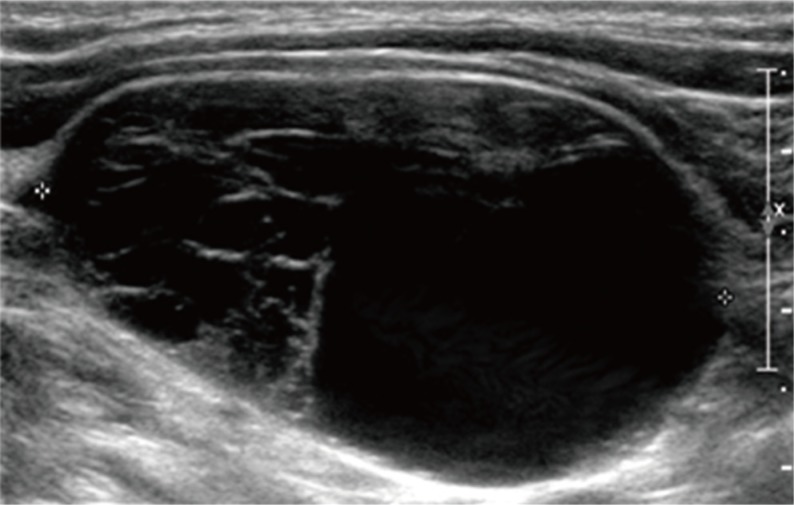
A Cervical Vagal Schwannoma Mimicking a Parathyroid Cyst
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon, Korea. lsw0922@schbc.ac.kr
- 2Department of Pathology, Soonchunhyang University College of Medicine, Bucheon, Korea.
Abstract
- Cervical vagal schwannomas with cystic degeneration changes are extremely rare. These tumors are typically benign and slow growing. A 44-year-old woman underwent complete resection of a tumor measuring 4x3.5 cm in the right neck using the endoscopic approach, instead of the conventional transcervical approach. We applied the new scarless neck surgery technique with an endoscopic unilateral axillo-breast approach. The tumor originated from the right vagus nerve, and was confirmed to be a vagal schwannoma pathologically. The patient has been followed up for 18 months postoperatively with no evidence of tumor recurrence or neurological deficit. We report an extremely rare vagal schwannoma with cystic degeneration that was removed by an endoscopic approach, along with a review of the relevant literature.
Figure
Reference
-
1. Chiofalo MG, Longo F, Marone U, Franco R, Petrillo A, Pezzullo L. Cervical vagal schwannoma: a case report. Acta Otorhinolaryngol Ital. 2009; 2. 29(1):33–35. PMID: 19609380.2. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; 6. 83(6):875. PMID: 8696772.
Article3. Park KT, Chang DY, Sung MW. Juvenile hyaline fibromatosis. Clin Exp Otorhinolaryngol. 2010; 6. 3(2):102–106. PMID: 20607080.
Article4. Chang SC, Schi YM. Neurilemmoma of the vagus nerve: a case report and brief literature review. Laryngoscope. 1984; 7. 94(7):946–949. PMID: 6738275.
Article5. Colreavy MP, Lacy PD, Hughes J, Bouchier-Hayes D, Brennan P, O'Dwyer AJ, et al. Head and neck schwannomas: a 10 year review. J Laryngol Otol. 2000; 2. 114(2):119–124. PMID: 10748827.6. Park KT, Ahn Y, Kim KH, Kwon TK. Schwannoma mimicking laryngocele. Clin Exp Otorhinolaryngol. 2010; 9. 3(3):166–171. PMID: 20978630.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tibial Schwannoma Mimicking a Popliteal Cyst
- A Case of Lymphoepithelial Cyst Mimicking Cervical Plexus Schwannoma
- Mediastinal parathyroid cyst: 1 case report
- Functional Parathyroid Cyst: A case report
- Cystic Giant Sacral Schwannoma Mimicking Aneurysmal Bone Cyst : A Case Report and Review of Literatures