A New Anterior Approach for Fluoroscopy-guided Suprascapular Nerve Block: A Preliminary Report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. kmshin1@yahoo.co.kr
- KMID: 2278151
- DOI: http://doi.org/10.3344/kjp.2012.25.3.168
Abstract
- BACKGROUND
The aim of the study was to investigate the feasibility of fluoroscopy-guided anterior approach for suprascapular nerve block (SSNB).
METHODS
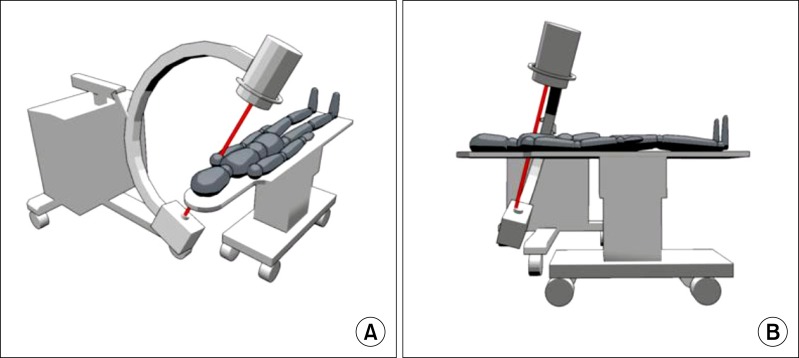
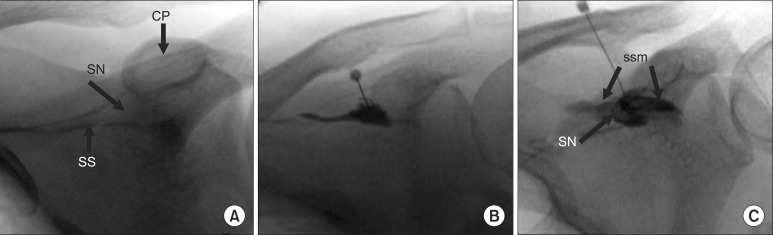
Twenty patients with chronic shoulder pain were included in the study. All of the nerve blocks were performed with patients in a supine position. Fluoroscopy was tilted medially to obtain the best view of the scapular notch (medial angle) and caudally to put the base of coracoid process and scapular spine on same line (caudal angle). SSNB was performed by introducing a 100-mm, 21-gauge needle to the scapular notch with tunnel view technique. Following negative aspiration, 1.0 ml of contrast was injected to confirm the scapular notch, and 1 % mepivacaine 2 ml was slowly injected. The success of SSNB was assessed by numerical rating scale (NRS) before and after the block.
RESULTS
The average NRS was decreased from 4.8 +/- 0.6 to 0.6 +/- 0.5 after the procedure (P < 0.05). The best view of the scapular notch was obtained in a medial angle of 15.1 +/- 2.2 (11-19degrees) and a caudal angle of 15.4 +/- 1.7degrees (12-18degrees). The average distance from the skin to the scapular notch was 5.8 +/- 0.6 cm. None of the complications such as pneumothorax, intravascular injection, and hematoma formation was found except one case of partial brachial plexus block.
CONCLUSIONS
SSNB by fluoroscopy-guided anterior approach is a feasible technique. The advantage of using a fluoroscopy resulted in an effective block with a small dose of local anesthetics by an accurate placement of a tip of needle in the scapular notch while avoiding pneumothorax.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Is Fluoroscopy-guided Suprascapular Nerve Block Better Than Other Techniques?
Jae Hang Shim
Korean J Pain. 2013;26(1):102-103. doi: 10.3344/kjp.2013.26.1.102.Acute Systemic Infusion of Bupropion Decrease Formalin Induced Pain Behavior in Rat
Somayyeh Naderi, Firouz Ghaderi Pakdel, Mostafa Ashrafi Osalou, Ulker Cankurt
Korean J Pain. 2014;27(2):118-124. doi: 10.3344/kjp.2014.27.2.118.Feasibility of Early and Repeated Low-dose Interscalene Brachial Plexus Block for Residual Pain in Acute Cervical Radiculopathy Treated with NSAIDS
Toshio Iwata, Mari Mitoro, Naoya Kuzumoto
Korean J Pain. 2014;27(2):125-132. doi: 10.3344/kjp.2014.27.2.125.Accuracy of suprascapular notch cross-sectional area by MRI in the diagnosis of suprascapular nerve entrapment syndrome: a retrospective pilot study
Jiyeon Park, Min-Ying Su, Young Uk Kim
Korean J Anesthesiol. 2022;75(6):496-501. doi: 10.4097/kja.22153.
Reference
-
1. Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003; 62:400–406. PMID: 12695149.
Article2. Emery P, Bowman S, Wedderburn L, Grahame R. Suprascapular nerve block for chronic shoulder pain in rheumatoid arthritis. BMJ. 1989; 299:1079–1080. PMID: 2511970.
Article3. Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. J Rheumatol. 2000; 27:1464–1469. PMID: 10852272.4. Granirer LW. A simple technic for suprascapular nerve block. N Y State J Med. 1951; 51:1048. PMID: 14827131.5. Moore DC. Regional block. 1965. 4th ed. Springfield, Ill.: Thomas;p. 300–303.6. Waldman SD. Waldman SD, editor. Suprascapular nerve block. Atlas of interventional pain management. 2004. 2nd ed. Philadelphia: Saunders;p. 163–165.
Article7. Gado K, Emery P. Modified suprascapular nerve block with bupivacaine alone effectively controls chronic shoulder pain in patients with rheumatoid arthritis. Ann Rheum Dis. 1993; 52:215–218. PMID: 8484675.
Article8. Kim CS, Lim KJ, Chung CD, Lee EY. The analgesic effect of continuous suprascapular nerve block after arthroscopic shoulder surgery. Korean J Anesthesiol. 2004; 47:92–95.
Article9. Hawkins RJ, Bokor DJ. Rockwood CA, Matsen FA, editors. Clinical evaluation of shoulder problems. The shoulder. 1998. 2nd ed. Philadelphia: Saunders;p. 164–197.10. Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996; (330):202–207. PMID: 8804294.
Article11. Feigl GC, Anderhuber F, Dorn C, Pipam W, Rosmarin W, Likar R. Modified lateral block of the suprascapular nerve: a safe approach and how much to inject? A morphological study. Reg Anesth Pain Med. 2007; 32:488–494. PMID: 18035294.
Article12. Schneider-Kolsky ME, Pike J, Connell DA. CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol. 2004; 33:277–282. PMID: 14872290.
Article13. Brown DL, Bridenbaugh LD. Cousins MJ, Bridenbaugh PO, editors. The upper extremity somatic block. Neural blockade in clinical anesthesia and management of pain. 1998. 3rd ed. Philadelphia: Lippincott-Raven;p. 345–371.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Blind and Ultasonography Guided Approach of Suprascapular Nerve Block
- The Proximal Approach in an Ultrasound-Guided Suprascapular Nerve Block
- Is Fluoroscopy-guided Suprascapular Nerve Block Better Than Other Techniques?
- Fluoroscopy-guided pudendal nerve block and pulsed radiofrequency treatment : A case report
- Ultrasound-Guided Intervention in Lumbar Spine