J Korean Orthop Assoc.
2017 Dec;52(6):521-528. 10.4055/jkoa.2017.52.6.521.
The Proximal Approach in an Ultrasound-Guided Suprascapular Nerve Block
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University Hospital, Daejeon, Korea.
- 2Hanmaeum Orthopaedic Clinic, Daejeon, Korea. borameos@hanmail.net
- KMID: 2421345
- DOI: http://doi.org/10.4055/jkoa.2017.52.6.521
Abstract
- PURPOSE
The purpose of this study was to analyze any effectiveness, advantages, and the procedure of an ultrasound-guided suprascapular nerve block via the proximal approach in patients suffering from shoulder pain.
MATERIALS AND METHODS
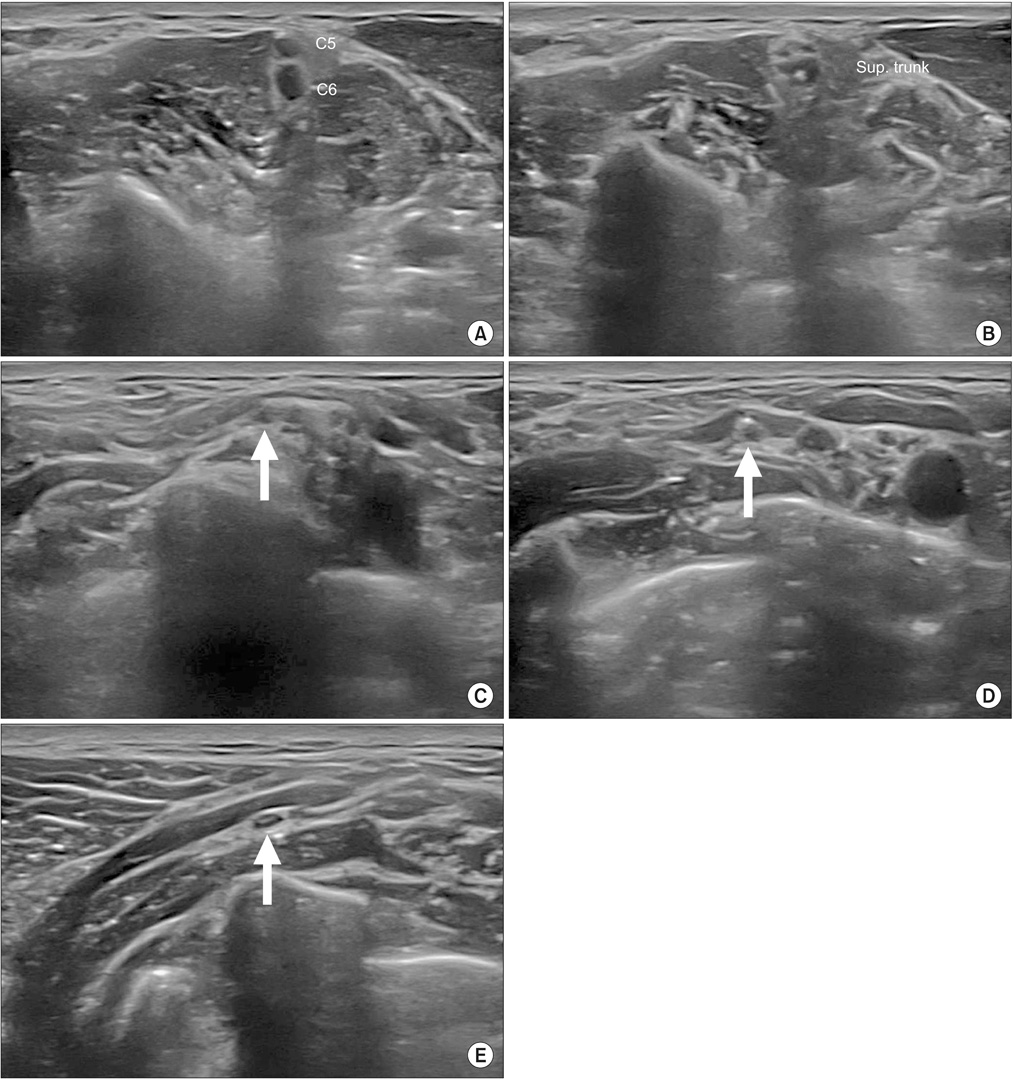
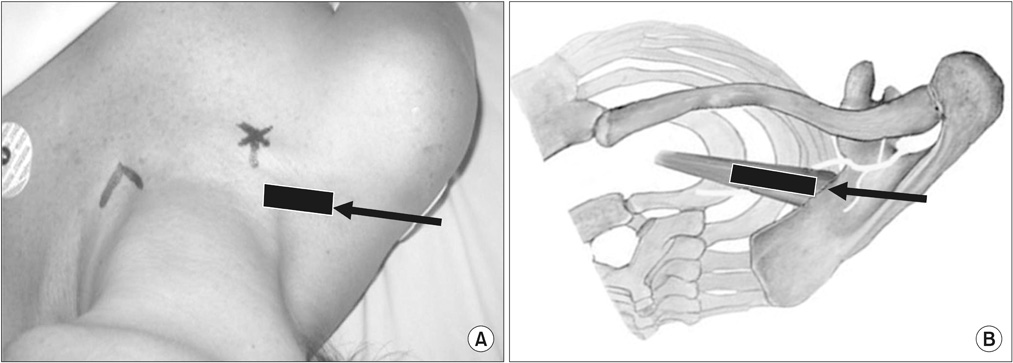
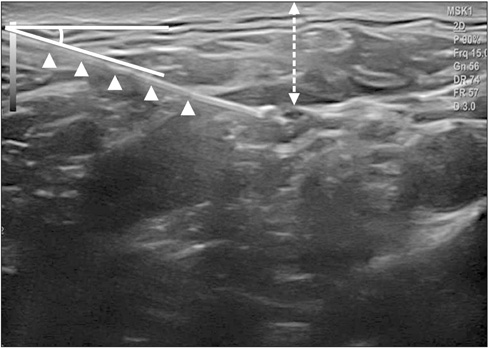
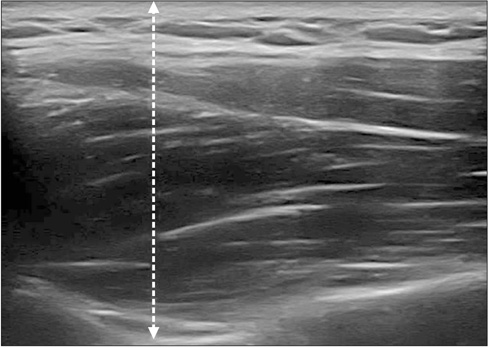
A total of 51 patients treated with nerve block between November 2015 and November 2016 were analyzed. We identified the suprascapular nerve that branches off the superior trunk of the brachial plexus, and found the suprascapular nerve, which is located in the fascial layer between the inferior belly of the omohyoid muscle and the serratus anterior muscle. We then performed a nerve block. We evaluated the visual analogue scale (VAS) of pre- and post-nerve block, and the visualization of the nerve, depth from the skin to the nerve, angle of needle entry, as well as complications. Moreover, we measured the visualization of the nerve, depth from the skin to the nerve in a classic approach, and compared it with the proximal approach.
RESULTS
There was significant improvement (p < 0.05) in the mean VAS, from 7.1 to 3.4, without any major complications. Compared with the classic approach, we were able to identify the suprascapular nerve much better (classic 25.5%/proximal 96.1%), and the mean distance from the skin to the nerve (classic 38 mm/proximal 12 mm) was significantly short (p < 0.05), and the mean angle of needle entry was 19 degrees in the proximal approach.
CONCLUSION
In an ultrasound-guided suprascapular nerve block by proximal approach, the nerve and needle tip can be more easily identified, which increases accuracy; with a small amount of local anesthetic, more effective pain control can be achieved. Hence, this approach is an effective alternative pain control method for patients suffering from shoulder pain.
Figure
Reference
-
1. Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. J Rheumatol. 2000; 27:1464–1469.2. Chang KV, Hung CY, Wang TG, Yang RS, Sun WZ, Lin CP. Ultrasound-guided proximal suprascapular nerve block with radiofrequency lesioning for patients with malignancy-associated recalcitrant shoulder pain. J Ultrasound Med. 2015; 34:2099–2105.
Article3. Lee SM, Park SE, Nam YS, et al. Analgesic effectiveness of nerve block in shoulder arthroscopy: comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc. 2012; 20:2573–2578.
Article4. Elsharkawy HA, Abd-Elsayed AA, Cummings KC 3rd, Soliman LM. Analgesic efficacy and technique of ultrasound-guided suprascapular nerve catheters after shoulder arthroscopy. Ochsner J. 2014; 14:259–263.5. Moon YL, Kang JH, Kim HH. The effectiveness of ultrasonography-guided suprascapular nerve block in patients treated with arthroscopic rotator cuff repair. J Korean Orthop Ultrasound Soc. 2014; 7:84–88.6. Harmon D, Hearty C. Ultrasound-guided suprascapular nerve block technique. Pain Physician. 2007; 10:743–746.7. Peng PW, Wiley MJ, Liang J, Bellingham GA. Ultrasound-guided suprascapular nerve block: a correlation with fluoroscopic and cadaveric findings. Can J Anesth. 2010; 57:143–148.
Article8. Vorster W, Lange CP, Briët RJ, et al. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elbow Surg. 2008; 17:500–502.
Article9. Siegenthaler A, Moriggl B, Mlekusch S, et al. Ultrasound-guided suprascapular nerve block, description of a novel supraclavicular approach. Reg Anesth Pain Med. 2012; 37:325–328.
Article10. Rothe C, Steen-Hansen C, Lund J, Jenstrup MT, Lange KH. Ultrasound-guided block of the suprascapular nerve: a volunteer study of a new proximal approach. Acta Anaesthesiol Scand. 2014; 58:1228–1232.11. Hackworth RJ. A new and simplified approach to target the suprascapular nerve with ultrasound. J Clin Anesth. 2013; 25:347–348.
Article12. Chan CW, Peng PW. Suprascapular nerve block: a narrative review. Reg Anesth Pain Med. 2011; 36:358–373.13. Taskaynatan MA, Ozgul A, Aydemir K, Koroglu OO, Tan AK. Accuracy of ultrasound-guided suprascapular nerve block measured with neurostimulation. Rheumatol Int. 2012; 32:2125–2128.
Article14. Fernandes MR, Barbosa MA, Sousa AL, Ramos GC. Suprascapular nerve block: important procedure in clinical practice. Part II. Rev Bras Reumatol. 2012; 52:616–622.15. Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality. Anesth Analg. 1997; 84:1306–1312.16. Neal JM, McDonald SB, Larkin KL, Polissar NL. Suprascapular nerve block prolongs analgesia after nonarthroscopic shoulder surgery but does not improve outcome. Anesth Analg. 2003; 96:982–986.
Article17. Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004; 99:589–592.
Article18. Jerosch J, Saad M, Greig M, Filler T. Suprascapular nerve block as a method of preemptive pain control in shoulder surgery. Knee Surg Sports Traumatol Arthrosc. 2008; 16:602–607.
Article19. Jeske HC, Kralinger F, Wambacher M, et al. A randomized study of the effectiveness of suprascapular nerve block in patient satisfaction and outcome after arthroscopic subacromial decompression. Arthroscopy. 2011; 27:1323–1328.
Article20. Lee JJ, Kim DY, Hwang JT, et al. Effect of ultrasonographically guided axillary nerve block combined with suprascapular nerve block in arthroscopic rotator cuff repair: a randomized controlled trial. Arthroscopy. 2014; 30:906–914.
Article21. Ozyuvaci E, Akyol O, Sitilci T, et al. Preoperative ultrasound-guided suprascapular nerve block for postthoracotomy shoulder pain. Curr Ther Res Clin Exp. 2013; 74:44–48.22. Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996; 330:202–207.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Blind and Ultasonography Guided Approach of Suprascapular Nerve Block
- Proximal Approach of Ultrasound-guided Suprascapular Nerve Block: Comparison with Subacromial Steroid Injection
- Ultrasound-Guided Intervention in Lumbar Spine
- The Efficacy of Ultrasound-Guided Lower Extremity Nerve Block in Trauma Patients
- Bilateral variant locations of the musculocutaneous nerve during ultrasound-guided bilateral axillary brachial plexus block: A case report