Korean J Obstet Gynecol.
2011 Aug;54(8):459-463. 10.5468/KJOG.2011.54.8.459.
Placental mesenchymal dysplasia associated with severe preeclampsia: A case report
- Affiliations
-
- 1Department of Obstetrics and Gynecology, CHA Gangnam Medical Center, CHA University, Seoul, Korea. jlee3575@hanmail.net
- 2Department of Pathology, CHA Gangnam Medical Center, CHA University, Seoul, Korea.
- KMID: 2274067
- DOI: http://doi.org/10.5468/KJOG.2011.54.8.459
Abstract
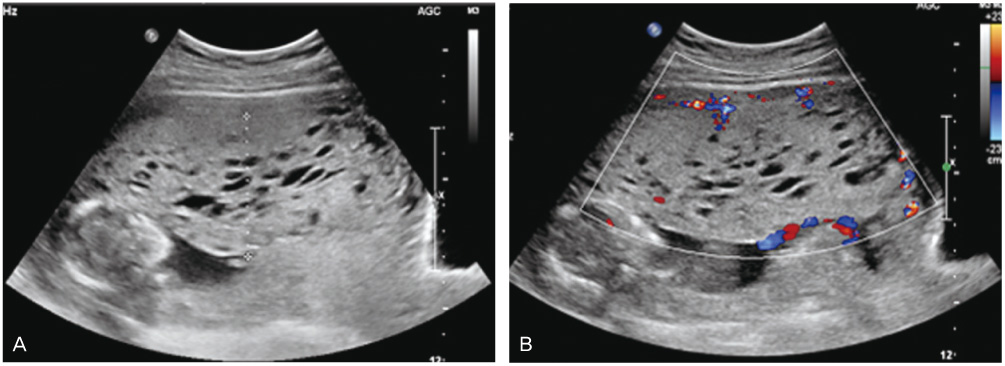
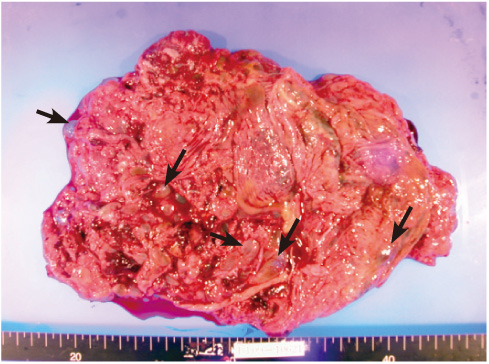
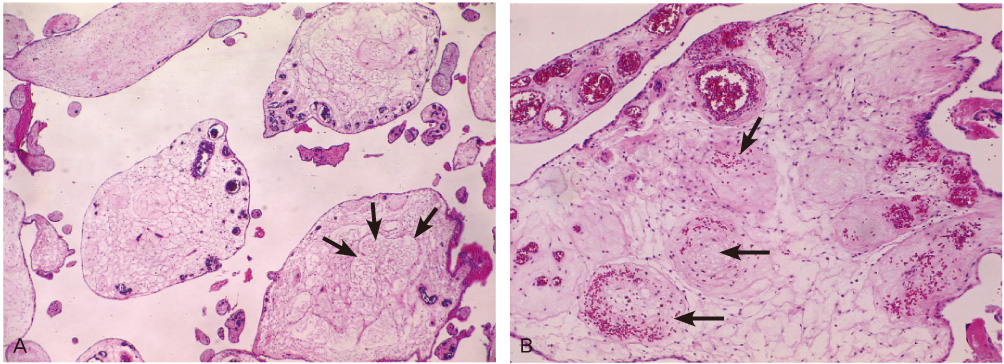
- Placental mesenchymal dysplasia (PMD) is a relatively recently recognized, rare placental vascular anomaly characterized by placentomegaly and grapelike vesicles that may coexist with a normal fetus. Ultrasonography performed at 16 weeks of gestation revealed multiple cysts in the placenta along with a morphologically normal fetus. At 24 weeks of gestational age, severe preeclampsia symptoms were seen. And sonographically intrauterine growth restriction (IUGR) and oligohydroamnios were noted. Based on the diagnosis of severe preeclampsia, termination of pregnancy was done. After termination, histopathologic examination of the placenta showed numerous grape-like cystic vesicles throughout the entire placenta and absence of trophoblastic proliferation and pseudoinclusions. We have described a pregnancy complicated with PMD associated with mid-trimester severe preeclampsia, IUGR and oligohydroamnios.
Figure
Reference
-
1. Moscoso G, Jauniaux E, Hustin J. Placental vascular anomaly with diffuse mesenchymal stem villous hyperplasia. A new clinico-pathological entity? Pathol Res Pract. 1991. 187:324–328.2. Feinberg RF, Kliman HJ, Cohen AW. Preeclampsia, trisomy 13, and the placental bed. Obstet Gynecol. 1991. 78:505–508.3. Kuwabara Y, Shima Y, Araki T, Shin S. Mesenchymal stem villous hyperplasia of the placenta and fetal growth restriction. Obstet Gynecol. 2001. 98:940–943.4. Jauniaux E, Nicolaides KH, Hustin J. Perinatal features associated with placental mesenchymal dysplasia. Placenta. 1997. 18:701–706.5. Pham T, Steele J, Stayboldt C, Chan L, Benirschke K. Placental mesenchymal dysplasia is associated with high rates of intrauterine growth restriction and fetal demise: A report of 11 new cases and a review of the literature. Am J Clin Pathol. 2006. 126:67–78.6. Arizawa M, Nakayama M. Suspected involvement of the X chromosome in placental mesenchymal dysplasia. Congenit Anom (Kyoto). 2002. 42:309–317.7. Müngen E, Dundar O, Muhcu M, Haholu A, Tunca Y. Placental mesenchymal dysplasia associated with trisomy 13: sonographic findings. J Clin Ultrasound. 2008. 36:454–456.8. Carta M, Maresi E, Giuffrè M, Catalano G, Piro E, Siracusa F, et al. Congenital hepatic mesenchymal hamartoma associated with mesenchymal stem villous hyperplasia of the placenta: case report. J Pediatr Surg. 2005. 40:e37–e39.9. Chen CP. Placental abnormalities and preeclampsia in trisomy 13 pregnancies. Taiwan J Obstet Gynecol. 2009. 48:3–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placental Mesenchymal Dysplasia Associated with Placenta Previa and Preterm Labor
- Maternal Preeclampsia and Bronchopulmonary Dysplasia
- Placental Mesenchymal Dysplasia Associated with a Fetal Unilateral Multicystic Dysplastic Kidney: A Case Report
- New Trends of Preeclampsia
- Midtrimester maternal plasma concentrations of angiopoietin 1, angiopoietin 2, and placental growth factor in pregnant women who subsequently develop preeclampsia