Korean J Obstet Gynecol.
2011 Aug;54(8):435-440. 10.5468/KJOG.2011.54.8.435.
High risk type human papillomavirus indicates increasing high grade intraepithelial lesion incidence in cytological low grade squamous intraepithelial lesion patients
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Hallym University College of Medicine, Chuncheon, Korea. drparkyh@yahoo.co.kr
- KMID: 2274063
- DOI: http://doi.org/10.5468/KJOG.2011.54.8.435
Abstract
OBJECTIVE
Human papillomavirus (HPV) is known as the causal agent of cervical cancer. The Papanicolaou smear is the most popular screening tool for cervical cancer. Some cytological low grade squamous intraepithelial lesions (LSILs) are in the developmental stage of high grade intraepithelial lesions (HSILs) and cervical cancer metaphases. Our purpose is to disclose the significance of high risk type (HRT) HPV in LSIL.
METHODS
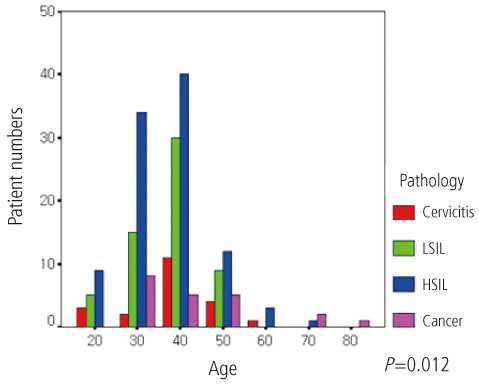
Documentation of 200 cases of cone biopsy at Hallym University Sacred Heart Hospital from February 2006 to February 2008 was reviewed retrospectively. HPV typing with DNA microarray results were found in 20 of the LSIL patients. Chi-square and student-t tests were used in the statistical analysis.
RESULTS
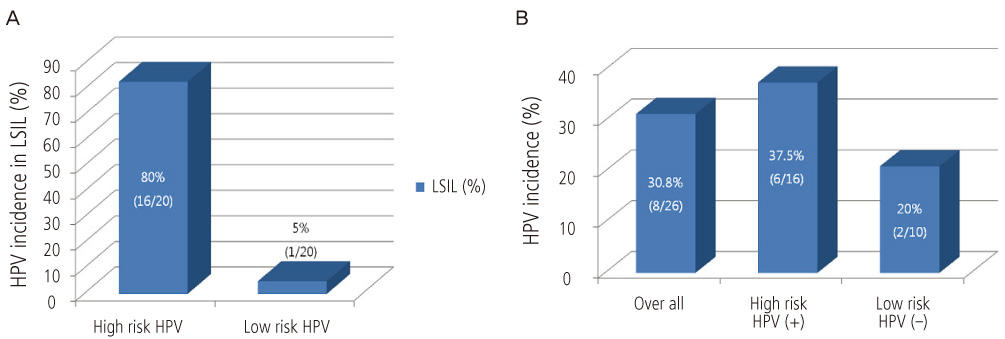
In the cytological LSIL patients, HRT-HPV positive patients were 16/20 (80%) and one low risk type (LRT) HPV positive patient was 1/20 (5%). In the cytological LSIL patients, postoperative pathological diagnoses were cervical intraepithelial neoplasia 1 (CIN 1) 16/26 (61.5%), CIN2 2/26 (7.7%), CIN3 5/26 (19.2%), carcinoma in situ 1/26 (3.8%). Among the 16 HRT-HPV positive patients, there were six that were above HSIL 6/16 (37.5%) in pathologic diagnoses. In the HRT-HPV negative 10 cytologic LSIL patients, there were two that were above HSIL 2/10 (20%) in pathologic diagnoses. HRT-HPV prevalences were not significantly different between LSIL and HSIL.
CONCLUSION
In HRT-HPV positive LSIL, the risk of HSIL or cancer of the cervix seems to be increasing. The HPV test is helpful in LSIL patient strategies and should be done in LSIL patients in order to discriminate between the nature and prognosis of cytological LSIL.
MeSH Terms
Figure
Reference
-
1. Sulik SM, Kroeger K, Schultz JK, Brown JL, Becker LA, Grant WD. Are fluid-based cytologies superior to the conventional Papanicolaou test? A systematic review. J Fam Pract. 2001. 50:1040–1046.2. Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006. 118:957–962.3. Ronco G, Segnan N, Giorgi-Rossi P, Zappa M, Casadei GP, Carozzi F, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006. 98:765–774.4. Mitchell MF, Tortolero-Luna G, Wright T, Sarkar A, Richards-Kortum R, Hong WK, et al. Cervical human papillomavirus infection and intraepithelial neoplasia: a review. J Natl Cancer Inst Monogr. 1996. 17–25.5. ter Haar-van Eck SA, Rischen-Vos J, Chadha-Ajwani S, Huikeshoven FJ. The incidence of cervical intraepithelial neoplasia among women with renal transplant in relation to cyclosporine. Br J Obstet Gynaecol. 1995. 102:58–61.6. ter Harmsel B, Smedts F, Kuijpers J, van Muyden R, Oosterhuis W, Quint W. Relationship between human papillomavirus type 16 in the cervix and intraepithelial neoplasia. Obstet Gynecol. 1999. 93:46–50.7. Solomon D, Schiffman M, Tarone R. ALTS Study group. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst. 2001. 93:293–299.8. Cox JT, Schiffman M, Solomon D. ASCUS-LSIL Triage Study (ALTS) Group. Prospective follow-up suggests similar risk of subsequent cervical intraepithelial neoplasia grade 2 or 3 among women with cervical intraepithelial neoplasia grade 1 or negative colposcopy and directed biopsy. Am J Obstet Gynecol. 2003. 188:1406–1412.9. Park TW, Fujiwara H, Wright TC. Molecular biology of cervical cancer and its precursors. Cancer. 1995. 76:1902–1913.10. Wright TC Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. Am J Obstet Gynecol. 2007. 197:340–345.11. The Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesions Triage Study (ALTS) Group. Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intraepithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst. 2000. 92:397–402.12. Moscicki AB, Schiffman M, Kjaer S, Villa LL. Chapter 5: Updating the natural history of HPV and anogenital cancer. Vaccine. 2006. 24:Suppl 3. S342–51.13. Moscicki AB, Hills N, Shiboski S, Powell K, Jay N, Hanson E, et al. Risks for incident human papillomavirus infection and low-grade squamous intraepithelial lesion development in young females. JAMA. 2001. 285:2995–3002.14. Sherman ME, Schiffman M, Cox JT. Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesion Triage Study Group. Effects of age and human papilloma viral load on colposcopy triage: data from the randomized Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesion Triage Study (ALTS). J Natl Cancer Inst. 2002. 94:102–107.15. Evans MF, Adamson CS, Papillo JL, St John TL, Leiman G, Cooper K. Distribution of human papillomavirus types in ThinPrep Papanicolaou tests classified according to the Bethesda 2001 terminology and correlations with patient age and biopsy outcomes. Cancer. 2006. 106:1054–1064.16. Schlecht NF, Platt RW, Duarte-Franco E, Costa MC, Sobrinho JP, Prado JC, et al. Human papillomavirus infection and time to progression and regression of cervical intraepithelial neoplasia. J Natl Cancer Inst. 2003. 95:1336–1343.17. Nobbenhuis MA, Helmerhorst TJ, van den Brule AJ, Rozendaal L, Voorhorst FJ, Bezemer PD, et al. Cytological regression and clearance of high-risk human papillomavirus in women with an abnormal cervical smear. Lancet. 2001. 358:1782–1783.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of Human Papillomavius DNA by Hybrid Capture Test in Cervical Intraepithelial Neoplasia and Carcinoma
- Effect of human papillomavirus genotype on severity and prognosis of cervical intraepithelial neoplasia
- Cervical intraepithelial neoplasia 3, coinfected with HPV-16 and -18: case report
- Visual inspection with acetic acid for detection of high grade lesion in atypical squamous cells and low grade squamous intraepithelial lesions from cervical Pap smear
- Endocervical Glandular Lesions in Invasive and Intraepithelial Squamous Neoplasms of the Uterine Cervix