Korean J Obstet Gynecol.
2011 Aug;54(8):420-427. 10.5468/KJOG.2011.54.8.420.
Characteristics of the pelvic floor during pregnancy by 2D and 3D ultrasound
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Guro Hospital, Korea University College of Medicine, Seoul, Korea. mjohmd@korea.ac.kr
- 2Department of Obstetrics and Gynecology, Ansan Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 2274061
- DOI: http://doi.org/10.5468/KJOG.2011.54.8.420
Abstract
OBJECTIVE
The aim of this study was to evaluate morphological characteristics of the pelvic floor in pregnant women using 2- and 3-dimensional (D)-transperineal ultrasound and compare our findings with findings in non-pregnant women.
METHODS
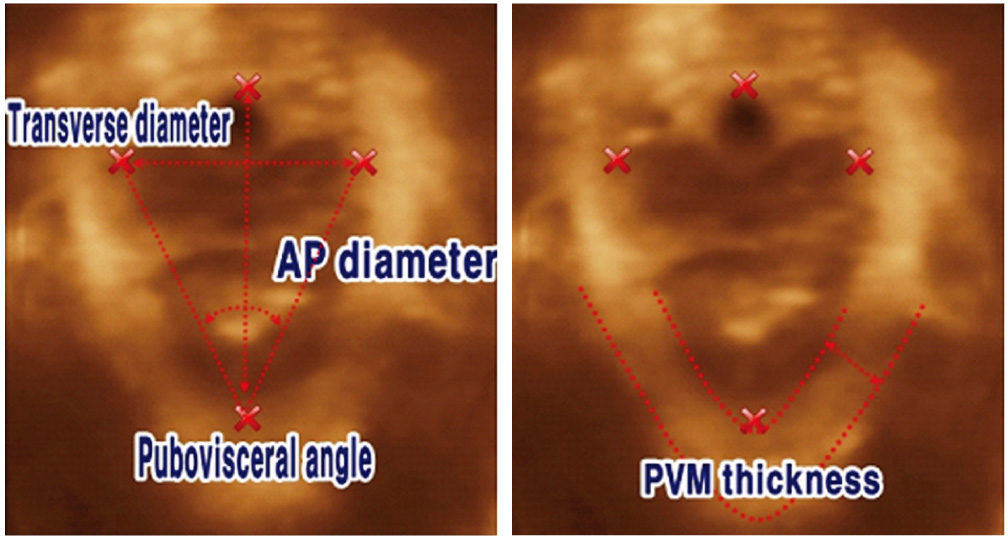
This case-control study included 40 nulliparous pregnant women at term and 28 nulliparous, non-pregnant women (age-matched). The 2D- and 3D-transperineal ultrasounds were carried out in the semi-supine position, after voiding, at rest and during the Valsalva maneuver. Various biometric parameters related to characteristics of the pelvic floor were measured.
RESULTS
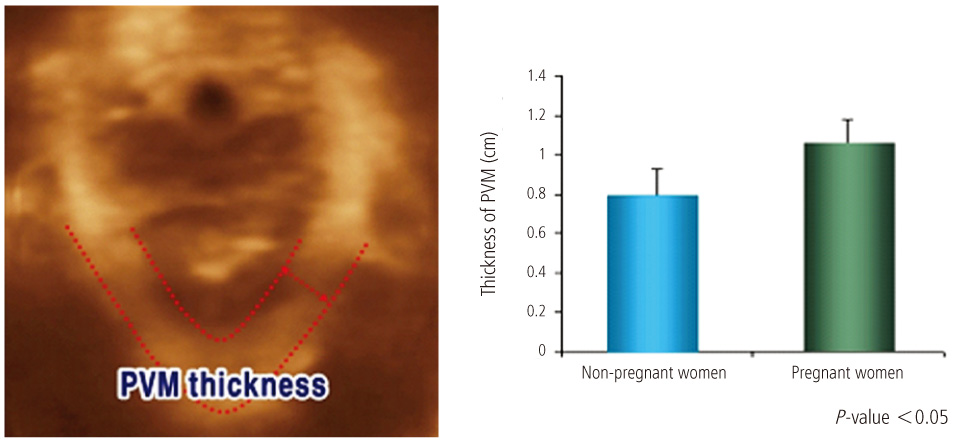
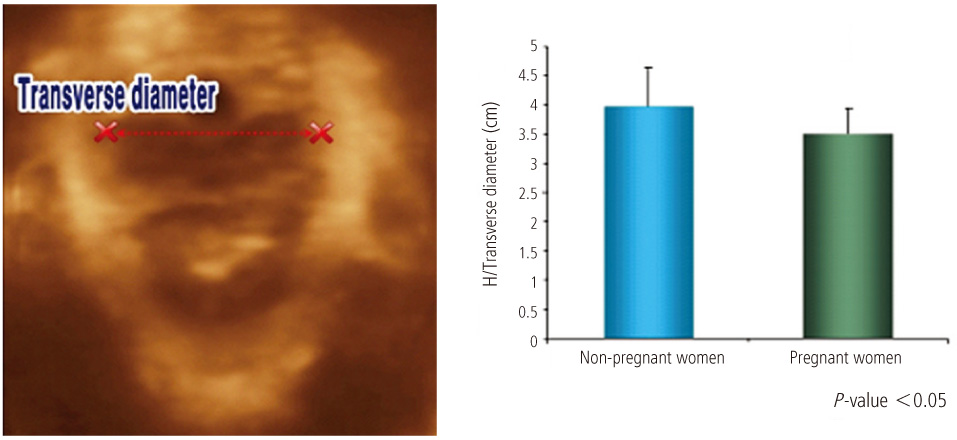
Satisfactory biometric measurements were obtained in all cases. The mean thickness of the levator ani muscle was significantly greater in pregnant women than in non-pregnant women (P<0.05). The mean levator hiatus angle and transverse diameter of the levator hiatus were significantly lower in pregnant women than in non-pregnant women (P<0.05). The anteroposterior diameter of the levator hiatus was not significantly different between pregnant women and non-pregnant women.
CONCLUSION
Pregnant women had significantly thicker the levator ani muscles but smaller hiatal areas, as measured by the levator hiatus angle and transverse diameter, than did non-pregnant women. Pregnancy itself may cause morphological changes to the pelvic floor to support the birth canal by closing the lower end of the pelvic cavity as a diaphragm. Further studies are needed to evaluate morphologic changes of the pelvic floor following delivery as measured by 2D and 3D-transperineal ultrasound.
Keyword
MeSH Terms
Figure
Reference
-
1. Fielding JR. Practical MR imaging of female pelvic floor weakness. Radiographics. 2002. 22:295–304.2. Singh K, Reid WM, Berger LA. Magnetic resonance imaging of normal levator ani anatomy and function. Obstet Gynecol. 2002. 99:433–438.3. Walters MD, Newton ER. Walters MD, Karram MM, editors. Pathophysiology and obstetric issues of genuine stress incontinence and pelvic floor dysfunction. Urogynecology and reconstructive pelvic surgery. 1999. 2nd ed. St. Louis: Mosby;135–144.4. Maubon A, Aubard Y, Berkane V, Camezind-Vidal MA, Marès P, Rouanet JP. Magnetic resonance imaging of the pelvic floor. Abdom Imaging. 2003. 28:217–225.5. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ. Williams obstetrics. 2009. 23rd ed. New York: McGraw-Hill Professional.6. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003. 101:46–53.7. Dietz HP, Haylen BT, Broome J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol. 2001. 18:511–514.8. Dietz HP. Levator function before and after childbirth. Aust N Z J Obstet Gynaecol. 2004. 44:19–23.9. Margulies RU, Hsu Y, Kearney R, Stein T, Umek WH, DeLancey JO. Appearance of the levator ani muscle subdivisions in magnetic resonance images. Obstet Gynecol. 2006. 107:1064–1069.10. Mørkved S, Salvesen KA, Bø K, Eik-Nes S. Pelvic floor muscle strength and thickness in continent and incontinent nulliparous pregnant women. Int Urogynecol J Pelvic Floor Dysfunct. 2004. 15:384–389.11. Falkert A, Endress E, Weigl M, Seelbach-Göbel B. Three-dimensional ultrasound of the pelvic floor 2 days after first delivery: influence of constitutional and obstetric factors. Ultrasound Obstet Gynecol. 2010. 35:583–588.12. Schaer G, Koelbl H, Voigt R, Merz E, Anthuber C, Niemeyer R, et al. Recommendations of the German Association of Urogynecology on functional sonography of the lower female urinary tract. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:105–108.13. Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005. 25:580–585.14. Schaer GN, Koechli OR, Schuessler B, Haller U. Perineal ultrasound: determination of reliable examination procedures. Ultrasound Obstet Gynecol. 1996. 7:347–352.15. Mouritsen L, Bach P. Ultrasonic evaluation of bladder neck position and mobility: the influence of urethral catheter, bladder volume, and body position. Neurourol Urodyn. 1994. 13:637–646.16. Tunn R, Petri E. Introital and transvaginal ultrasound as the main tool in the assessment of urogenital and pelvic floor dysfunction: an imaging panel and practical approach. Ultrasound Obstet Gynecol. 2003. 22:205–213.17. Dietz HP, Wilson PD. The influence of bladder volume on the position and mobility of the urethrovesical junction. Int Urogynecol J Pelvic Floor Dysfunct. 1999. 10:3–6.18. Tunn R, Schaer G, Peschers U, Bader W, Gauruder A, Hanzal E, et al. Updated recommendations on ultrasonography in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct. 2005. 16:236–241.19. Blatt AH, Titus J, Chan L. Ultrasound measurement of bladder wall thickness in the assessment of voiding dysfunction. J Urol. 2008. 179:2275–2278.20. Krofta L, Otcenásek M, Kasíková E, Feyereisl J. Pubococcygeuspuborectalis trauma after forceps delivery: evaluation of the levator ani muscle with 3D/4D ultrasound. Int Urogynecol J Pelvic Floor Dysfunct. 2009. 20:1175–1181.21. Costantini S, Nadalini C, Esposito F, Valenzano MM, Risso D, Lantieri P, et al. Perineal ultrasound evaluation of the urethrovesical junction angle and urethral mobility in nulliparous women and women following vaginal delivery. Int Urogynecol J Pelvic Floor Dysfunct. 2005. 16:455–459.22. Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:437–440.23. Dannecker C, Anthuber C. The effects of childbirth on the pelvic-floor. J Perinat Med. 2000. 28:175–184.24. Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007. 109:1396–1403.25. Viktrup L, Rortveit G, Lose G. Risk of stress urinary incontinence twelve years after the first pregnancy and delivery. Obstet Gynecol. 2006. 108:248–254.26. MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000. 107:1460–1470.27. Wijma J, Weis Potters AE, de Wolf BT, Tinga DJ, Aarnoudse JG. Anatomical and functional changes in the lower urinary tract during pregnancy. BJOG. 2001. 108:726–732.28. Wang LI, Ying LI. Effect of pregnancy on the pelvic floor muscle tonus. J Chinese Clin Med. 2009. 4:385–387.29. Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA. Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol. 2004. 103:31–40.30. Salvesen KA, Mørkved S. Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ. 2004. 329:378–380.31. Dietz HP. Ultrasound imaging of the pelvic floor. Part II: three-dimensional or volume imaging. Ultrasound Obstet Gynecol. 2004. 23:615–625.32. Lanzarone V, Dietz HP. Three-dimensional ultrasound imaging of the levator hiatus in late pregnancy and associations with delivery outcomes. Aust N Z J Obstet Gynaecol. 2007. 47:176–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anal canal coronal-sagittal ratio: a novel parameter for diagnosing pelvic floor injury in 2-dimensional transanal ultrasound
- Comparison of 3-Dimensional Pelvic Floor Ultrasonography and Defecography for Assessment of Posterior Pelvic Floor Disorders
- The Interobserver Variability and Diagnostic Performance of 3-Dimensional Breast Ultrasound
- Pelvic floor muscle rehabilitation
- Prenatally diagnosed split hand malformation at 16 weeks' gestation by 3D ultrasonography