Korean J Orthod.
2013 Dec;43(6):279-287. 10.4041/kjod.2013.43.6.279.
The predictability of dentoskeletal factors for soft-tissue chin strain during lip closure
- Affiliations
-
- 1Department of Orthodontics, Graduate School of Clinical Dentistry, Korea University, Seoul, Korea. estelle7@korea.ac.kr
- KMID: 2273421
- DOI: http://doi.org/10.4041/kjod.2013.43.6.279
Abstract
OBJECTIVE
To investigate the dentoskeletal factors which may predict soft-tissue chin strain during lip closure.
METHODS
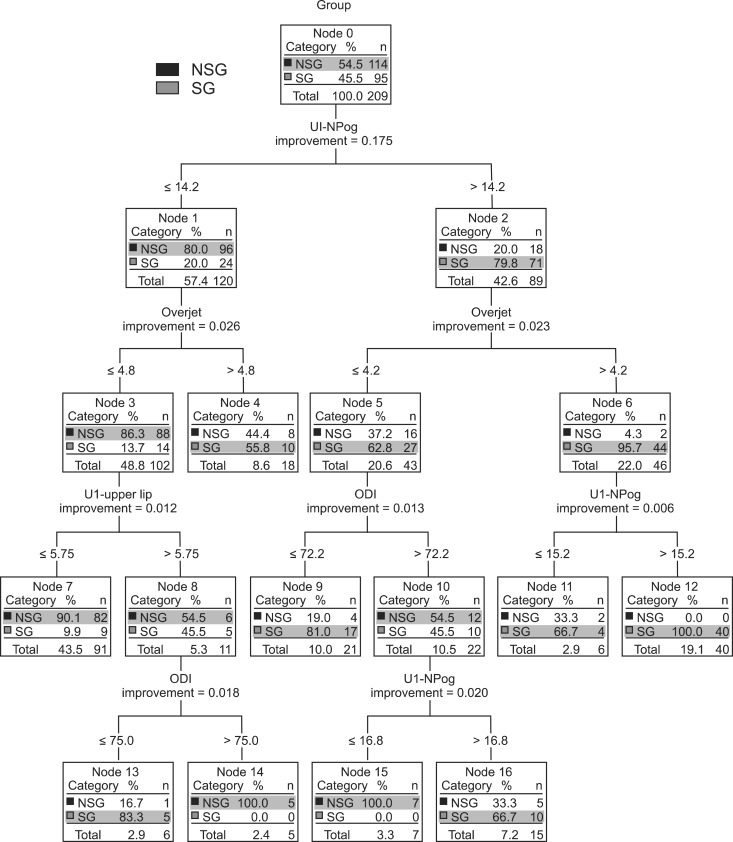
The pretreatment frontal and lateral facial photographs and lateral cephalograms of 209 women (aged 18-30 years) with Angle's Class I or II malocclusion were examined. The subjects were categorized by three examiners into the no-strain and strain groups according to the soft-tissue chin tension or deformation during lip closure. Relationships of the cephalometric measurements with the group classification were analyzed by logistic regression analysis, and a classification and regression tree (CART) model was used to define the predictive variables for the group classification.
RESULTS
The lower the value of the overbite depth indicator (ODI) and the higher the values of upper incisor to Nasion-Pogonion (U1-NPog, mm), overjet, and upper incisor to upper lip (U1-upper lip, mm), the more likely was the subject to be classified into the strain group. The CART showed that U1-NPog was the most prominent predictor of soft-tissue chin strain (cut-off value of 14.2 mm), followed by overjet.
CONCLUSIONS
To minimize strain of the soft-tissue chin, orthodontic treatment should be oriented toward increasing the ODI value while decreasing the U1-NPog, overjet, and U1 upper lip values.
Figure
Reference
-
1. Subtelny JD. A longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structures. Am J Orthod. 1959; 45:481–507.
Article2. Burstone CJ. Lip posture and its significance in treatment planning. Am J Orthod. 1967; 53:262–284. PMID: 5227460.
Article3. Yogosawa F. Predicting soft tissue profile changes concurrent with orthodontic treatment. Angle Orthod. 1990; 60:199–206. PMID: 2389852.4. Zide BM, McCarthy J. The mentalis muscle: an essential component of chin and lower lip position. Plast Reconstr Surg. 1989; 83:413–420. PMID: 2645595.
Article5. Dewan SK, Marjadi UK. Soft tissue changes in surgically treated cases of bimaxillary protrusion. J Oral Maxillofac Surg. 1983; 41:116–118. PMID: 6571879.
Article6. Fisher MA, Wenger RM, Hans MG. Pretreatment characteristics associated with orthodontic treatment duration. Am J Orthod Dentofacial Orthop. 2010; 137:178–186. PMID: 20152672.
Article7. Kneafsey LC, Cunningham SJ, Petrie A, Hutton TJ. Prediction of soft-tissue changes after mandibular advancement surgery with an equation developed with multivariable regression. Am J Orthod Dentofacial Orthop. 2008; 134:657–664. PMID: 18984398.
Article8. Loh WY. Classification and regression trees. Wiley Interdiscip Rev Data Min Knowl Discov. 2011; 1:14–23.
Article9. Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. New York: Wadsworth, Inc;1984.10. Hambleton RS. The soft-tissue covering of the skeletal face as related to orthodontic problems. Am J Orthod. 1964; 50:405–420.
Article11. Nishida N, Tanaka M, Hayashi N, Nagata H, Takeshita T, Nakayama K, et al. Determination of smoking and obesity as periodontitis risks using the classification and regression tree method. J Periodontol. 2005; 76:923–928. PMID: 15948686.
Article12. Park M, Choi S, Shin AM, Koo CH. Analysis of the characteristics of the older adults with depression using data mining decision tree analysis. J Korean Acad Nurs. 2013; 43:1–10. PMID: 23563063.
Article13. Banovic I, Gilibert D, Jebrane A, Cosnes J. Diagnostic profiles determined by the C.A.R.T procedure: IBD patients and fatigue. J Health Psychol. 2012; 17:500–508. PMID: 21963682.
Article14. Lee YJ, Park YG. Correlations between muscle activities of orbicularis oris, mentalis, buccinator and suprahyoid and craniofacial morphology in Class II division 1 malocclusion with incompetent lips and normal occlusion. Korean J Orthod. 1994; 24:199–220.15. James RD. A comparative study of facial profiles in extraction and nonextraction treatment. Am J Orthod Dentofacial Orthop. 1998; 114:265–276. PMID: 9743131.
Article16. Han UA, Kim JH, Yoon TH, Park JU, Kook YA. Hard and soft tissue profile changes following anterior subapical osteotomy in bimaxillary dentoalveolar protrusion patients. Korean J Orthod. 2003; 33:475–483.17. Otuyemi OD. Lower lip position and incisor overjet in a 12-year-old Nigerian population. Afr Dent J. 1993; 7:27–30. PMID: 9590877.18. Otuyemi OD. Variability in upper lip posture to overjet changes in 12-year-old Nigerian children. Afr Dent J. 1996; 10:33–36. PMID: 9590892.19. Hayashida H, Ioi H, Nakata S, Takahashi I, Counts AL. Effects of retraction of anterior teeth and initial soft tissue variables on lip changes in Japanese adults. Eur J Orthod. 2011; 33:419–426. PMID: 20966067.
Article20. Cao L, Zhang K, Bai D, Jing Y, Tian Y, Guo Y. Effect of maxillary incisor labiolingual inclination and anteroposterior position on smiling profile esthetics. Angle Orthod. 2011; 81:121–129. PMID: 20936964.
Article21. Paula DF Jr, Silva ÉT, Campos AC, Nuñez MO, Leles CR. Effect of anterior teeth display during smiling on the self-perceived impacts of malocclusion in adolescents. Angle Orthod. 2011; 81:540–545. PMID: 21261487.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A roentgenocephalometric study of profile changes in orthodontically treated patients
- The Role of Various Osseous Genioplasty Combined with Orthoganthic Surgery
- Augmentation of the Chin with a Silicone Implant
- A longitudintal study of soft-tissue profile changes in Korean adults aged from 24 to 32 years
- Prediction of Soft Tissue Profile Changes after Mandibular Set-back Surgery