Korean J Orthod.
2010 Apr;40(2):95-105. 10.4041/kjod.2010.40.2.95.
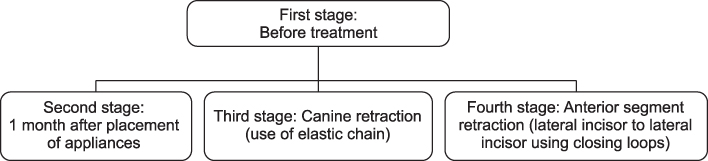
Changes in the oral environment during four stages of orthodontic treatment
- Affiliations
-
- 1Department of Orthodontics, Research Center, School of Dentistry, Universidad Autonoma del Estado de Mexico, Toluca, Estado de Mexico, Mexico.
- 2Research Center, School of Dentistry, Universidad Autonoma del Estado de Mexico, Toluca, Estado de Mexico, Mexico. montiel74@hotmail.com
- 3Health Attention Department, Universidad Autonoma Metropolitana, Unidad Xochimilco, Mexico City, Mexico.
- 4Research Center, School of Dentistry, Universidad Autonoma del Estado de Mexico, Toluca, Estado de Mexico, Mexico.
- KMID: 2273217
- DOI: http://doi.org/10.4041/kjod.2010.40.2.95
Abstract
OBJECTIVE
To identify clinical, salivary, and bacterial changes during orthodontic treatment with follow-up to 24 months.
METHODS
In 30 patients, clinical (decayed, missing, and filled surfaces [DMFS], O'Leary's plaque index, and plaque pH), salivary (unstimulated and stimulated saliva, buffer capacity, pH, and occult blood), and bacterial (Streptococcus mutans and Lactobacillus) markers were evaluated. A questionnaire was employed to evaluate their hygienic-dietary habits. Data were analyzed by ANOVA, logistic regression and Spearman's correlation.
RESULTS
DMFS increased significantly, whereas the plaque index diminished, plaque pH was more acidic (p = 0.23), and unstimulated salivary flow showed significant differences during the treatment (p = 0.013). Stimulated saliva flow increased in females after the placement of appliances; buffer capacity was diminished in males during the therapy; salivary pH remained at basal values. Bacterial levels and occult blood increased to high-risk levels and were not statistically significant different between genders (p > 0.05). Two major relationships were confirmed: initial plaque with use of dental aids (r = 0.429; p = 0.018) and final DMFS with unstimulated salivary flow (r = -0.372; p = 0.043).
CONCLUSIONS
The increase in retentive surfaces increased the bacterial levels, plaque pH became acidified, and gingival damage was greater. Buffer capacity was altered but maintained a healthy salivary pH during the treatment.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Antimicrobial effect of different brushing frequencies with fluoride toothpaste on Streptococcus mutans and Lactobacillus species in children with fixed orthodontic appliances
Kristina Peros, Senka Mestrovic, Sandra Anic-Milosevic, Kata Rosin-Grget, Mladen Slaj
Korean J Orthod. 2012;42(5):263-269. doi: 10.4041/kjod.2012.42.5.263.
Reference
-
1. Rosenbloom RG, Tinanoff N. Salivary Streptococcus Mutans levels in patients before, during and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991. 100:35–37.
Article2. Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of Mutans Streptococci and Lactobacilli. Aust Orthod J. 1999. 15:229–234.3. Papaioannou W, Gizani S, Nassika M, Kontou E, Nakou M. Adhesion of Streptococcus Mutans to different types of brackets. Angle Orthod. 2007. 77:1090–1095.4. Yu JK, Ahn SJ, Lee SJ, Chang YI. Quantitative analysis of Mutans Streptococci adhesion to various orthodontic bracket materials in vivo. Korean J Orthod. 2009. 39:105–111.
Article5. Choi JH. Comparison of slim bristled and V-shaped orthodontic toothbrushes in patients with fixed orthodontic appliances. Korean J Orthod. 2009. 39:383–392.
Article6. Faltermeier A, Bürgers R, Rosentritt M. Bacterial adhesion of Streptococcus Mutans to esthetic bracket materials. Am J Orthod Dentofacial Orthop. 2008. 133:4 Suppl. S99–S103.7. Alves PV, Alviano WS, Bolognese AM, Nojima LI. Treatment protocol to control Streptococcus Mutans level in an orthodontic patient with high caries risk. Am J Orthod Dentofacial Orthop. 2008. 133:91–94.
Article8. Derks A, Kujipers-Jagtman AM, Frencken JE, Van't Hof MA, Katsaros C. Caries preventive measures used in orthodontic practices: An evidence-based decision? Am J Orthod Dentofacial Orthop. 2007. 132:165–170.
Article9. Sharma NC, Lyle DM, Qaqish JG, Galustians J, Schuller R. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2008. 133:565–571.
Article10. Costa MR, Silva VC, Miqui MN, Sakima T, Spolidorio DM, Cirelli JA. Efficacy of ultrasonic, electric and manual toothbrushes in patients with fixed orthodontic appliances. Angle Orthod. 2007. 77:361–366.
Article11. Tufekci E, Casagrande ZA, Lindauer SJ, Fowler CE, Williams KT. Effectiveness of an essential oil mouthrinse in improving oral health in orthodontic patients. Angle Orthod. 2008. 78:294–298.
Article12. Derks A, Frencken J, Bronkhorst E, Kuijpers-Jagtman AM, Katsaros C. Effect of chlorhexidine varnish application on Mutans Streptococci counts in orthodontic patients. Am J Orthod Dentofacial Orthop. 2008. 133:435–439.
Article13. World Health Organization. Oral Health Surveys. Basic methods. 1997. 3rd ed. Geneva: WHO.14. Arrieta-Blanco JJ, Bartolomé-Villar B, Jiménez-Martinez E, Saavedra-Vallejo P, Arrieta-Blanco FJ. Bucco-dental problems in patients with diabetes mellitus (I): Index of plaque and dental caries. Med Oral. 2003. 8:97–109.15. O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972. 43:38.16. Koroluk L, Hoover JN, Komiyama K. The sensitivity and specificity of a colorimetric microbiological caries activity test (Cariostat) in preschool children. Pediatr Dent. 1994. 16:276–281.17. Montiel BN, Satoh Y, Shimizu Y, Kawarai C, Kanegae H, Yasui T. Relationship among snack taking, caries activity, and caries prevalence in Japanese infants and young children. Meikai Univ Dent J. 2002. 31:149–153.18. Varma S, Banerjee A, Bartlett D. An in vivo investigation of associations between saliva properties, caries prevalence and potential lesion activity in an adult UK population. J Dent. 2008. 36:294–299.
Article19. Jensen B, Bratthall D. A new method for the estimation of Mutans Streptococci in human saliva. J Dent Res. 1989. 68:468–471.
Article20. Davenport ES, Day S, Hardie JM, Smith JM. A comparison between commercial kits and conventional methods for enumeration of salivary Mutans Streptococci and Lactobacilli. Community Dental Health. 1992. 9:261–271.21. Larmas M. A new dip-slide method for the counting of salivary Lactobacilli. Proc Finn Dent Soc. 1975. 71:31–35.22. Montiel BN, Nagai A. A study on changes in some oral environmental factors caused by orthodontic treatment with fixed appliances. Meikai Univ Dent J. 2006. 34:188–197.23. Farsi N. Dental caries in relation to salivary factors in Saudi population groups. J Contemp Dent Pract. 2008. 9:16–23.
Article24. Hickman J, Millett DT, Sander L, Brown E, Love J. Powered vs manual tooth brushing in fixed appliance patients: A short term randomized clinical trial. Angle Orthod. 2002. 72:135–140.25. Davies TM, Shaw WC, Worthington HV, Addy M, Dummer P, Kingdon A. The effect of orthodontic treatment on plaque and gingivitis. Am J Orthod Dentofacial Orthop. 1991. 99:155–161.
Article26. Percival RS, Challacombe SJ, Marsh PD. Flow rates of resting whole and stimulated parotid saliva in relation to age and gender. J Dent Res. 1994. 73:1416–1420.
Article27. de Almeida PV, Gregio AM, Machado MA, de Lima AA, Azevedo LR. Saliva composition and functions: a comprehensive review. J Contemp Dent Pract. 2008. 9:72–80.
Article28. Fenoll-Palomares C, Muñoz-Montagud JV, Sanchiz V, Herreros B, Hernández V, Mínguez M, et al. Unstimulated salivary flow rate, pH and buffer capacity of saliva in healthy volunteers. Rev Esp Enferm Dig. 2004. 96:773–783.
Article29. Nishimura M, Bhuiyan MM, Matsumura S, Shimono T. Assesment of the caries activity test (Cariostat) based on the infection levels of Mutans Streptococci and Lactobacilli in 2- to 13-year children's dental plaque. J Dent Child. 1988. 65:248–251.30. Smiech-Slomkowska G, Jablonska-Zrobek J. The effect of oral health education on dental plaque development and the level of caries-related Streptococcus Mutans and Lactobacillus spp. Eur J Orthod. 2007. 29:157–160.
Article31. Geiger AM. Malocclusion as an etiologic factor in periodontal disease: A retrospective essay. Am J Orthod Dentofacial Orthop. 2001. 120:112–115.
Article32. Hashimoto M, Yamanaka K, Shimosato T, Ozawa A, Takigawa T, Hidaka S, et al. Oral condition and health status of elderly 8020 achievers in Aichi Prefecture. Bull Tokyo Dent Coll. 2006. 47:37–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerable factors for final occlusion in pre-orthodontic lower anterior segmental surgery and its availability
- The Relationships between Orthodontic Treatment, Oral Health-Related Quality of Life, and Happiness of among Some High School Students
- Oral Impact on Daily Performance and Happiness related to Orthodontic Treatment of Some Middle and High School Students with Malocclusion
- Managing oral biofilms to avoid enamel demineralization during fixed orthodontic treatment
- Diagnosis and Treatment of Malocclusions using the Invisalign System