Korean J Orthod.
2009 Jun;39(3):185-198. 10.4041/kjod.2009.39.3.185.
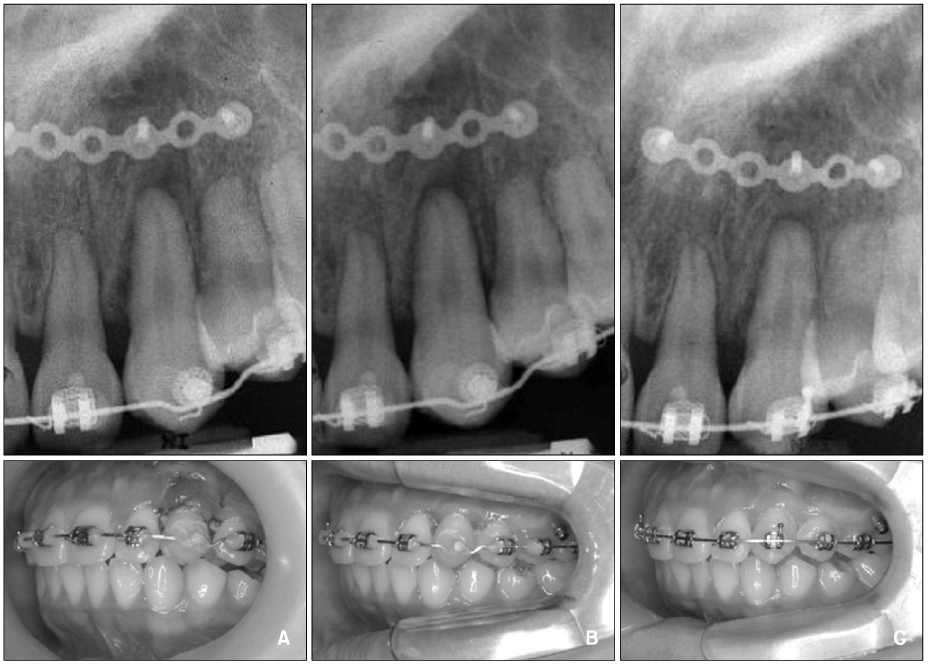
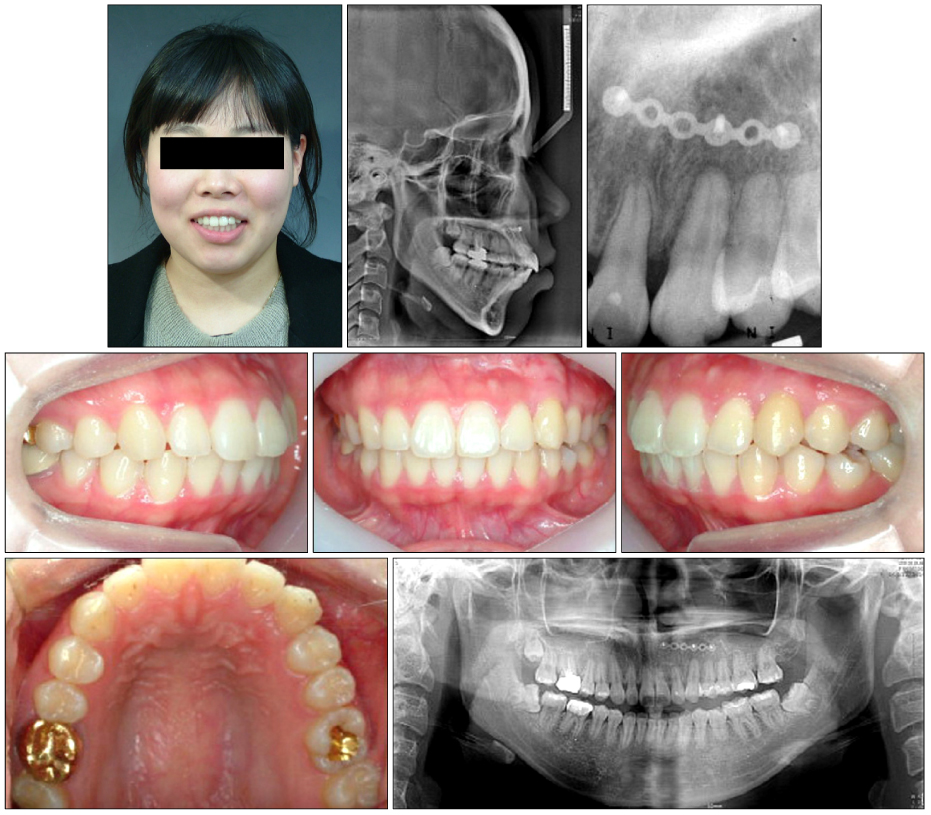
Orthodontic treatment of an ankylosed tooth; application of single tooth osteotomy and alveolar bone distraction osteogenesis
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Pusan National University, Busan, Korea. sbypark@pusan.ac.kr
- KMID: 2273213
- DOI: http://doi.org/10.4041/kjod.2009.39.3.185
Abstract
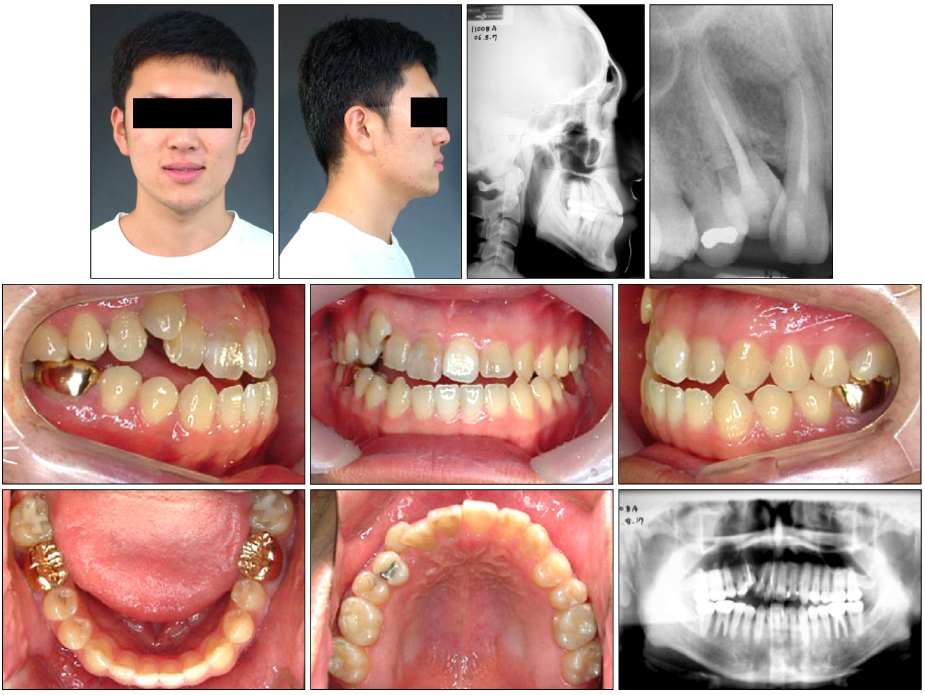
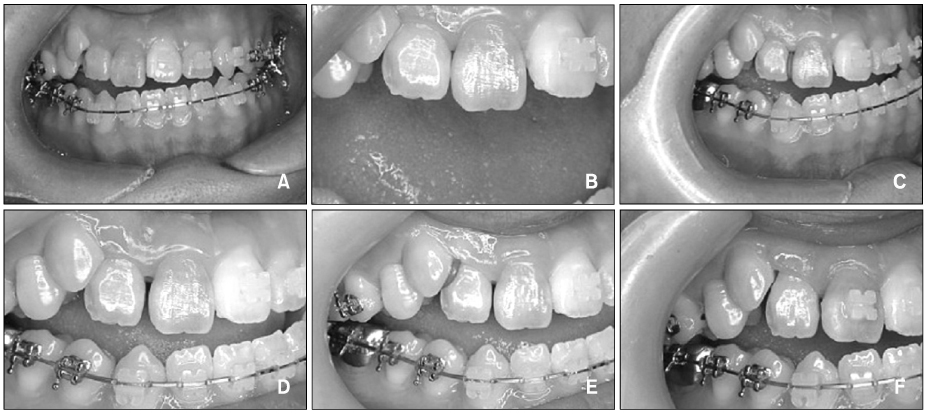
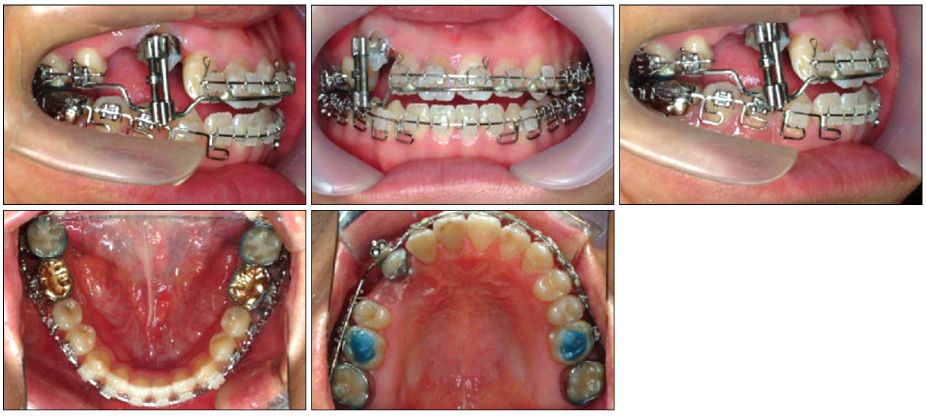
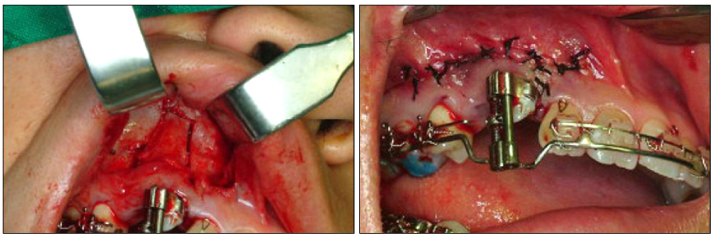
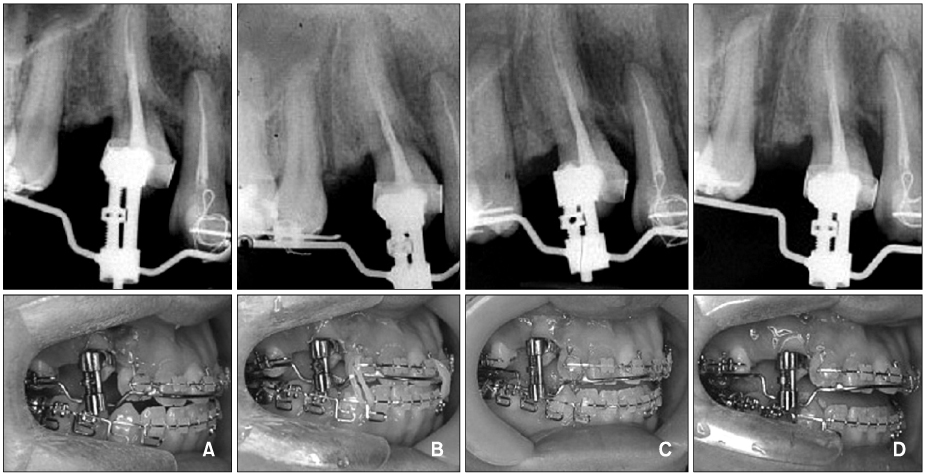
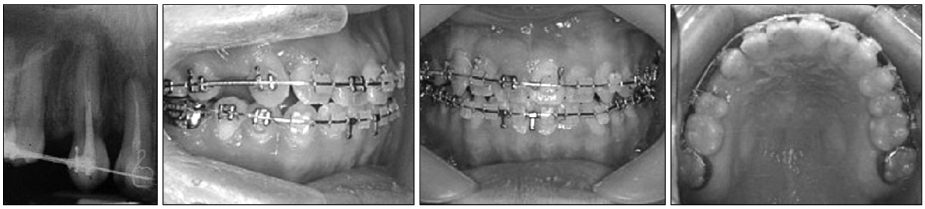
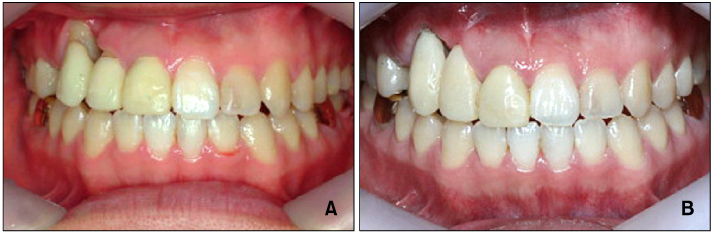
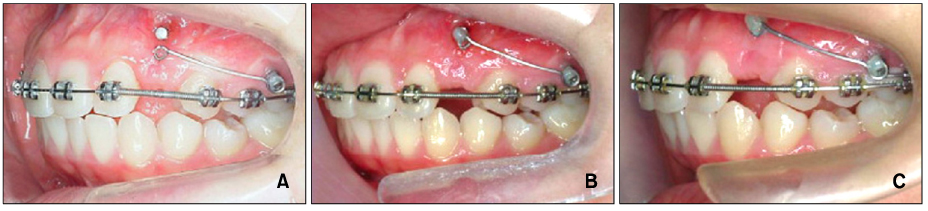
- Tooth anklylosis is defined as the adhesion state of alveolar bone to dentin or cementum. Trauma, disturbed metabolic disease, and congenital disease have been given as etiologic factors. Complications of tooth ankylosis are tipping of the neighboring teeth, space loss, and supraeruption of the opposing teeth. Particularly if dental ankylosis occurs in maxillary incisors of a growing child, the ankylosed tooth can not move vertically with subsequent disturbance in vertical growth of the alveolar process. With an appropriate treatment approach, an esthetic condition must be achieved especially in the maxillary anterior region. In this report, two cases are presented which were treated by the surgical repositioning method. One is treated by alveolar bone distraction osteogenesis which used a tooth-borne type distraction device and the other by single tooth osteotomy.
MeSH Terms
Figure
Reference
-
1. The Korean Council of the Faculty of Orthodontics. Textbook of orthodontics. 2006. Seoul: Daehannarae Publishing;150.2. Frazier-Bowers SA, Koehler KE, Ackerman JL, Proffit WR. Primary failure of eruption: Further characterization of a rare eruption disorder. Am J Orthod Dentofacial Orthop. 2007. 131:e1–e11.
Article3. Andreasen JO. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg. 1981. 10:54–61.
Article4. Biederman W. Etiology and treatment of tooth ankylosis. Am J Orthod. 1962. 48:670–684.
Article5. Kurol J, Thilander B. Infraocclusion of primary molars and the effect on occlusal development, a longitudinal study. Eur J Orthod. 1984. 6:277–293.
Article6. Alcan T. A miniature tooth-borne distractor for the alignment of ankylosed teeth. Angle Orthod. 2006. 76:77–83.7. Kofod T, Würtz V, Melsen B. Treatment of an ankylosed central incisor by single tooth dento-osseous osteotomy and a simple distraction device. Am J Orthod Dentofacial Orthop. 2005. 127:72–80.
Article8. Razdolsky Y, El-Bialy TH, Dessner S, Buhler JE Jr. Movement of ankylosed permanent teeth with a distraction device. J Clin Orthod. 2004. 38:612–620.9. Kinzinger GS, Jänicke S, Riediger D, Diedrich PR. Orthodontic fine adjustment after vertical callus distraction of an ankylosed incisor using the floating bone concept. Am J Orthod Dentofacial Orthop. 2003. 124:582–590.
Article10. Son WS, Chung IK, Shin SH. Surgically assisted orthodontic treatment of ankylosed maxillary incisor. Korean J Orthod. 2002. 32:257–264.11. Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990. 250:8–26.
Article12. McCarthy JG, Stelnicki EJ, Grayson BH. Distraction osteogenesis of the mandible: a ten-year experience. Semin Orthod. 1999. 5:3–8.13. Toth BA, Kim JW, Chin M, Cedars M. Distraction osteogenesis and its application to the midface and bony orbit in craniosynostosis syndromes. J Cranofac Surg. 1998. 9:100–113.
Article14. Samchukov ML, Cope JB, Cherkashin AM. Craniofacial distraction osteogenesis. 2001. St. Louis: Mosby;379–458.15. Albers DD. Ankylosis of teeth in the developing dentition. Quintessence Int. 1986. 17:303–308.16. Hammarström L, Pierce A, Blomlöf L, Feiglin B, Lindskog S. Tooth avulsion and replantation - a review. Endod Dent Traumatol. 1986. 2:1–8.
Article17. Lindskog S, Pierce AM, Blomlof L, Hammarstrom L. The role of the necrotic periodontal membrane in cementum resorption and ankylosis. Endod Dent Traumatol. 1985. 1:96–101.
Article18. Malmgren B, Malmgren O. Rate of infraposition of reimplanted ankylosed incisors related to age and growth in children and adolescents. Dent Traumatol. 2002. 18:28–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Managements of ankylosed incisor occurred during adolescence using alveolar bone distraction osteogenesis and decoronation: case report
- Surgically assisted orthodontic treatment of ankylosed maxillary incisor
- Distraction Osteogenesis of Mandible using Short-Sagittal Osteotomy for the Patient with Hemifacial Microsomia
- Corticotomy and the Intrusive Tooth Movement
- Correction of a Wide Alveolar Cleft with Reverse L Osteotomy and Liou Alveolar Distractor