Korean J Orthod.
2012 Jun;42(3):144-154. 10.4041/kjod.2012.42.3.144.
Management of acquired open bite associated with temporomandibular joint osteoarthritis using miniscrew anchorage
- Affiliations
-
- 1Institute of Health Biosciences, The University of Tokushima Graduate School, Tokushima, Japan. etanaka@dent.tokushima-u.ac.jp
- 2Nonoyama Orthodontic Clinic, Higashihiroshima, Japan.
- 3Hiroshima University Graduate School of Biomedical Sciences, Hiroshima, Japan.
- KMID: 2272263
- DOI: http://doi.org/10.4041/kjod.2012.42.3.144
Abstract
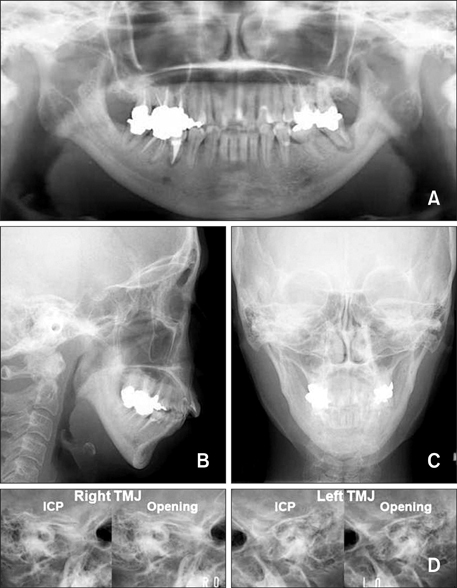
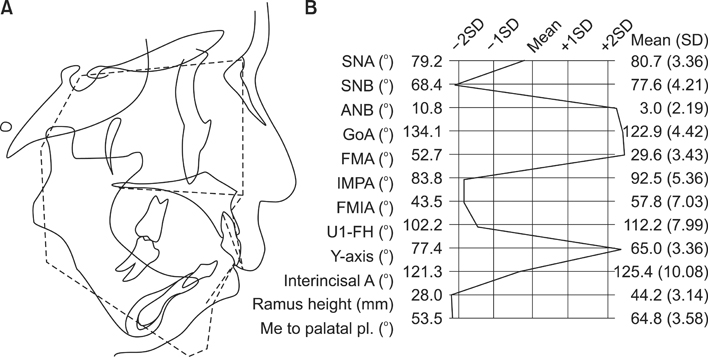
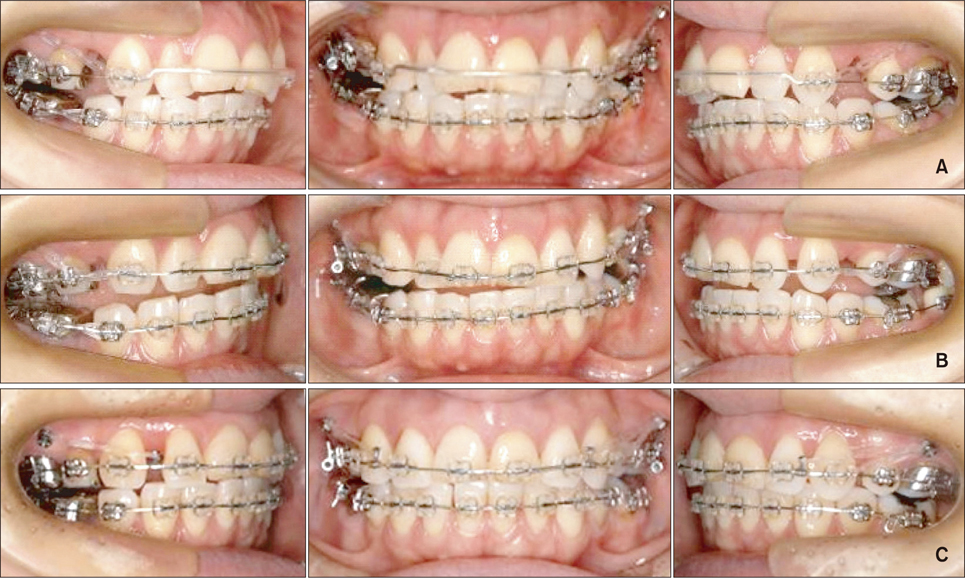
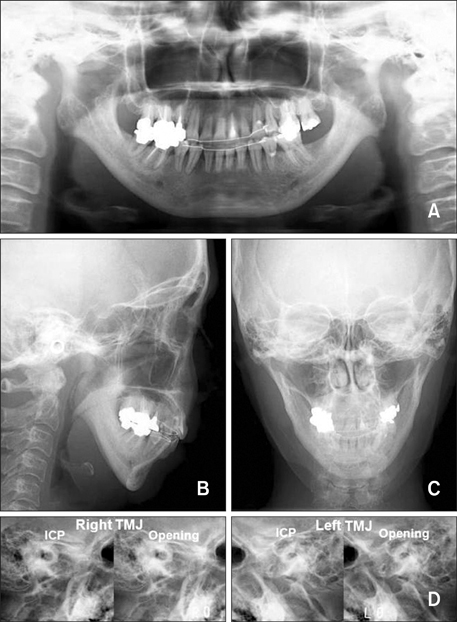
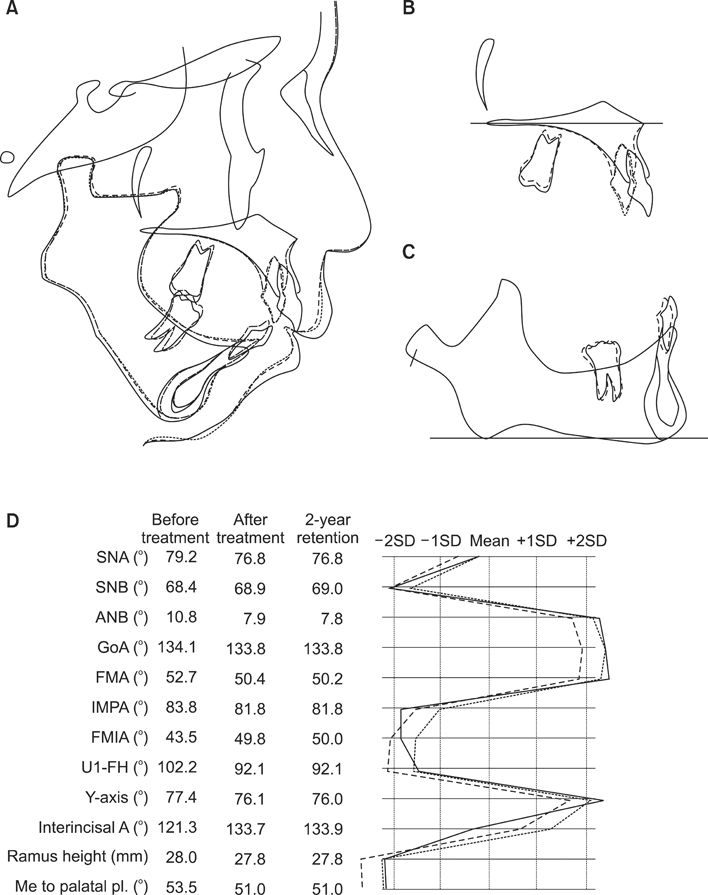
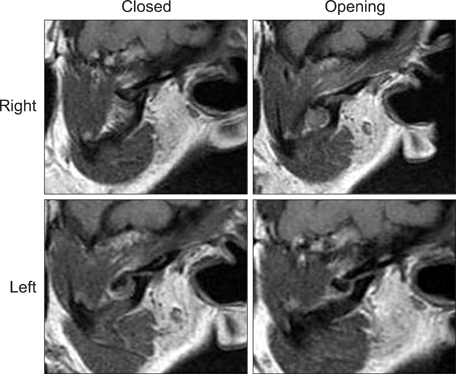
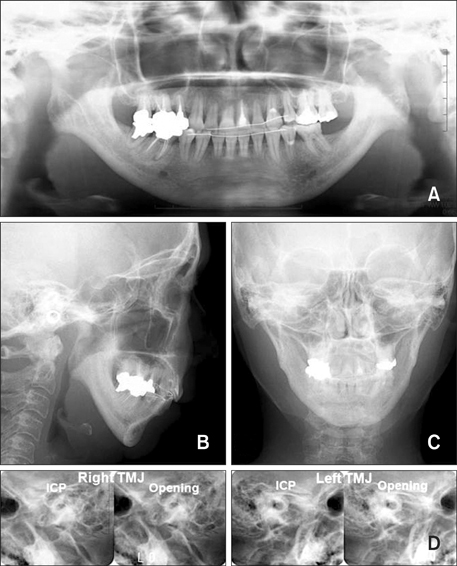
- This article reports the orthodontic treatment of a patient with skeletal mandibular retrusion and an anterior open bite due to temporomandibular joint osteoarthritis (TMJ-OA) using miniscrew anchorage. A 46-year-old woman had a Class II malocclusion with a retropositioned mandible. Her overjet and overbite were 7.0 mm and -1.6 mm, respectively. She had limited mouth opening, TMJ sounds, and pain. Condylar resorption was observed in both TMJs. Her TMJ pain was reduced by splint therapy, and then orthodontic treatment was initiated. Titanium miniscrews were placed at the posterior maxilla to intrude the molars. After 2 years and 7 months of orthodontic treatment, an acceptable occlusion was achieved without any recurrence of TMJ symptoms. The retropositioned mandible was considerably improved, and the lips showed less tension upon lip closure. The maxillary molars were intruded by 1.5 mm, and the mandible was subsequently rotated counterclockwise. Magnetic resonance imaging of both condyles after treatment showed avascular necrosis-like structures. During a 2-year retention period, an acceptable occlusion was maintained without recurrence of the open bite. In conclusion, correction of open bite and clockwise-rotated mandible through molar intrusion using titanium miniscrews is effective for the management of TMJ-OA with jaw deformity.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Treatment and retention of relapsed anterior open-bite with low tongue posture and tongue-tie: A 10-year follow-up
Yu-Jin Seo, Su-Jung Kim, Janchivdorj Munkhshur, Kyu-Rhim Chung, Peter Ngan, Seong-Hun Kim
Korean J Orthod. 2014;44(4):203-216. doi: 10.4041/kjod.2014.44.4.203.
Reference
-
1. Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. J Dent Res. 2008. 87:296–307.
Article2. Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996. 110:117–127.
Article3. Nitzan DW. The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: a theoretical concept. J Oral Maxillofac Surg. 2001. 59:36–45.
Article4. Laskin D. Etiology and pathogenesis of internal derangement of the temporomandibular joint (Current controversies in surgery for internal derangements of the temporomandibular joint). Oral Maxillofac Surg Clin North Am. 1994. 6:217–222.5. Kuroda S, Tanimoto K, Izawa T, Fujihara S, Koolstra JH, Tanaka E. Biomechanical and biochemical characteristics of the mandibular condylar cartilage. Osteoarthritis Cartilage. 2009. 17:1408–1415.
Article6. De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV, De Mot BM. Condylar resorption in orthognathic surgery: a retrospective study. Int J Adult Orthodon Orthognath Surg. 1994. 9:233–240.7. Crawford JG, Stoelinga PJ, Blijdorp PA, Brouns JJ. Stability after reoperation for progressive condylar resorption after orthognathic surgery: report of seven cases. J Oral Maxillofac Surg. 1994. 52:460–466.
Article8. Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg. 2003. 61:655–660.
Article9. Gonçalves JR, Cassano DS, Wolford LM, Santos-Pinto A, Márquez IM. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: affect of articular disc repositioning. J Oral Maxillofac Surg. 2008. 66:724–738.
Article10. Kuroda S, Katayama A, Takano-Yamamoto T. Severe anterior open-bite case treated using titanium screw anchorage. Angle Orthod. 2004. 74:558–567.11. Wada K, Otani S, Sakuda M. Yamauchi K, Sakuda M, editors. Morphometric analysis in maxillary protrusion. Maxillary Protrusion. 1989. Tokyo: Ishiyaku;95–130. [in Japanese].12. Magnusson T, Ahlborg G, Svartz K. Function of the masticatory system in 20 patients with mandibular hypo- or hyperplasia after correction by a sagittal split osteotomy. Int J Oral Maxillofac Surg. 1990. 19:289–293.
Article13. Moore KE, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: report of five cases. J Oral Maxillofac Surg. 1991. 49:448–460.
Article14. Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994. 52:2–10.
Article15. Tanaka E, Tanaka M, Watanabe M, Del Pozo R, Tanne K. Influences of occlusal and skeletal discrepancies on biomechanical environment in the TMJ during maximum clenching: an analytic approach with the finite element method. J Oral Rehabil. 2001. 28:888–894.
Article16. Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999. 115:166–174.
Article17. Kuroda S, Sugawara Y, Tamamura N, Takano-Yamamoto T. Anterior open bite with temporomandibular disorder treated with titanium screw anchorage: evaluation of morphological and functional improvement. Am J Orthod Dentofacial Orthop. 2007. 131:550–560.
Article18. Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007. 132:599–605.
Article19. Kuroda S, Tanaka E. Application of temporary anchorage devices for the treatment of adult Class III malocclusions. Semin Orthod. 2011. 17:91–97.
Article20. Tanaka E, Kikuchi K, Sasaki A, Tanne K. An adult case of TMJ osteoarthrosis treated with splint therapy and the subsequent orthodontic occlusal reconstruction: adaptive change of the condyle during the treatment. Am J Orthod Dentofacial Orthop. 2000. 118:566–571.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Open Bite with Temporomandibular Joint Osteoarthritis Treated with Skeletal Anchorage Device: A Case Report
- A study on the treatment of anterior open bite with midpalatal miniscrews
- Use of Intermaxillary Traction Appliances and Exercises to Strengthen the Masticatory Muscles of Patients with Anterior Open Bite Caused by Temporomandibular Joint Osteoarthritis: Case Reports
- Management of open bite that developed during treatment for internal derangement and osteoarthritis of the temporomandibular joint
- Anterior open bite with temporomandibular disorders treated with intermaxillary traction using skeletal anchorage system