Ann Surg Treat Res.
2014 Nov;87(5):253-259. 10.4174/astr.2014.87.5.253.
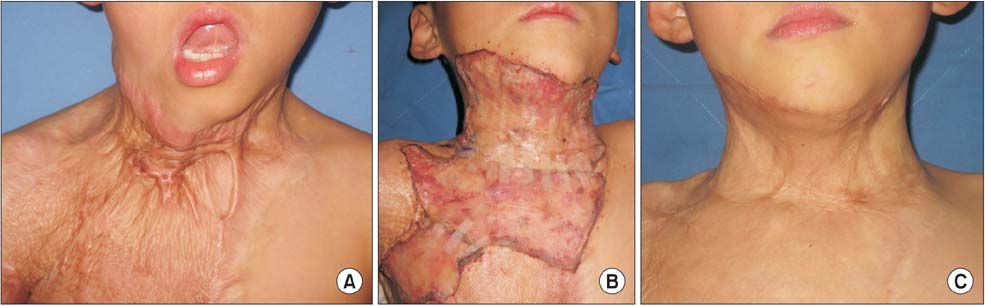
Management of neck contractures by single-stage dermal substitutes and skin grafting in extensive burn patients
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Burn Center, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea.
- 2Department of Surgery and Critical Care, Burn Center, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea. hammerj@hallym.or.kr
- KMID: 2266884
- DOI: http://doi.org/10.4174/astr.2014.87.5.253
Abstract
- PURPOSE
Severe neck contracture is a problem that must be resolved by priority. We consider the best contracture treatment to be the full-thickness skin graft. However, clinicians often encounter patients, especially extensive burn patients, who have insufficient donor sites for the full-thickness skin graft. We treated extensive burn patients with neck scar contractures with a split-thickness skin graft (STSG) combined with dermal substitutes. The purpose of this study was to evaluate clinical outcomes of neck contracture treatment in extensive burn patients performing STSG with dermal substitutes as adjuvant treatment.
METHODS
We analyzed the retrospective clinical and photographic records of 28 patients with severe neck contracture who were admitted to Hallym University Hangang Sacred Heart Hospital, Seoul, Korea, from January 2012 to December 2012. We performed STSG in combination with dermal substitutes to minimize the degree of contracture.
RESULTS
The overall take rate of skin to dermal substitutes was 95.9%, and no grafts failed to affect recontracture except in one patient with a partial loss of artificial dermis who underwent a follow-up skin graft without any problems. Excellent/good outcomes were shown in 27 out of 28 patients.
CONCLUSION
In extensive burn patients, skin grafting in combination with dermal substitutes can be an alternative to STSG alone for contracture release.
Keyword
MeSH Terms
Figure
Reference
-
1. Wetzig T, Gebhardt C, Simon JC. New indications for artificial collagen-elastin matrices? Covering exposed tendons. Dermatology. 2009; 219:272–273.2. Saaiq M, Zaib S, Ahmad S. The menace of post-burn contractures: a developing country's perspective. Ann Burns Fire Disasters. 2012; 25:152–158.3. Goel A, Shrivastava P. Post-burn scars and scar contractures. Indian J Plast Surg. 2010; 43:Suppl. S63–S71.4. Stiefel D, Schiestl C, Meuli M. Integra artificial skin for burn scar revision in adolescents and children. Burns. 2010; 36:114–120.5. Serghiou M, Cowan A, Whitehead C. Rehabilitation after a burn injury. Clin Plast Surg. 2009; 36:675–686.6. Neale HW, Billmire DA, Carey JP. Reconstruction following head and neck burns. Clin Plast Surg. 1986; 13:119–136.7. Moustafa MF, Borhan A, Abdel-Fattah , Abdel-Fattah . Burn contractures of the neck. Plast Reconstr Surg. 1978; 62:66–73.8. Wainwright DJ. Burn reconstruction: the problems, the techniques, and the applications. Clin Plast Surg. 2009; 36:687–700.9. Wainwright DJ, Bury SB. Acellular dermal matrix in the management of the burn patient. Aesthet Surg J. 2011; 31:7 Suppl. 13S–23S.10. van Zuijlen PP, van Trier AJ, Vloemans JF, Groenevelt F, Kreis RW, Middelkoop E. Graft survival and effectiveness of dermal substitution in burns and reconstructive surgery in a one-stage grafting model. Plast Reconstr Surg. 2000; 106:615–623.11. Sheridan RL, Moreno C. Skin substitutes in burns. Burns. 2001; 27:92.12. Walden JL, Garcia H, Hawkins H, Crouchet JR, Traber L, Gore DC. Both dermal matrix and epidermis contribute to an inhibition of wound contraction. Ann Plast Surg. 2000; 45:162–166.13. Wainwright DJ. Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns. 1995; 21:243–248.14. Rennekampff HO, Pfau M, Schaller HE. Acellular allograft dermal matrix: immediate or delayed epidermal coverage? Burns. 2002; 28:100–101.15. Ryssel H, Radu CA, Germann G, Otte M, Gazyakan E. Single-stage Matriderm and skin grafting as an alternative recon struction in high-voltage injuries. Int Wound J. 2010; 7:385–392.16. Haslik W, Kamolz LP, Nathschlager G, Andel H, Meissl G, Frey M. First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand. Burns. 2007; 33:364–368.17. Philandrianos C, Andrac-Meyer L, Mordon S, Feuerstein JM, Sabatier F, Veran J, et al. Comparison of five dermal substitutes in full-thickness skin wound healing in a porcine model. Burns. 2012; 38:820–829.18. Haslik W, Kamolz LP, Manna F, Hladik M, Rath T, Frey M. Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J Plast Reconstr Aesthet Surg. 2010; 63:360–364.19. Heimbach DM, Warden GD, Luterman A, Jordan MH, Ozobia N, Ryan CM, et al. Multicenter postapproval clinical trial of Integra dermal regeneration template for burn treatment. J Burn Care Rehabil. 2003; 24:42–48.20. Oh SJ, Kim Y. Combined AlloDerm and thin skin grafting for the treatment of postburn dyspigmented scar contracture of the upper extremity. J Plast Reconstr Aesthet Surg. 2011; 64:229–233.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of Matriderm(R) with Autologous Skin Graft in Full Thickness Burns
- Effectiveness of Thick Acellular Dermal Matrix (Allocover(R)) in Burn and Burn Scar Contracture
- Penile Skin Necrosis after Dermal fat Graft Augmentation
- The Capacity of 2 mm Matriderm(R) as a Dermal Substitute in Single Stage Skin Resurfacing
- Split-Thickness Skin Grafting with Meshed Matriderm(R) in Burn Wound Management