Ann Rehabil Med.
2011 Jun;35(3):354-360. 10.5535/arm.2011.35.3.354.
Reliability of Visual Classification of Sagittal Gait Patterns in Patients with Bilateral Spastic Cerebral Palsy
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute, Yonsei University College of Medicine, Seoul 120-752, Korea. medicus@yuhs.ac
- KMID: 2266854
- DOI: http://doi.org/10.5535/arm.2011.35.3.354
Abstract
OBJECTIVE
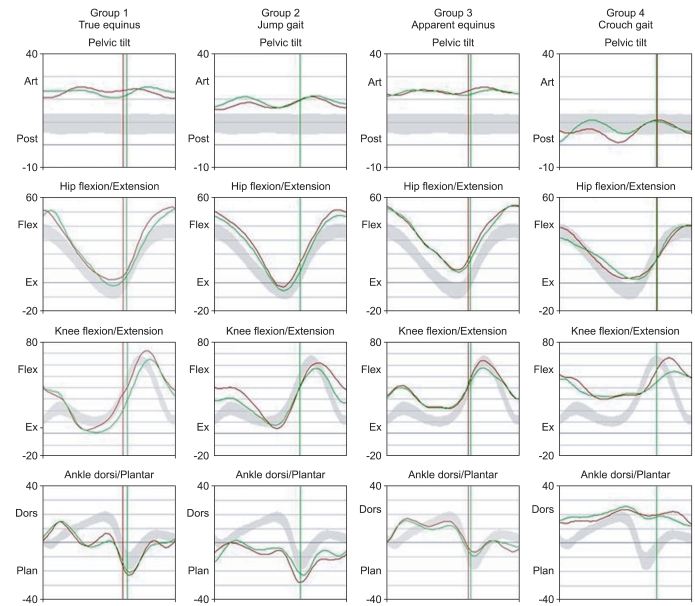
To investigate the reliability of inspection-based classification of sagittal gait patterns in children with bilateral spastic cerebral palsy (CP). METHOD: Video clip recordings of gait patterns and sagittal kinematic data obtained by a computerized motion analysis system from 91 patients with bilateral spastic CP were reviewed. The abnormal gait patterns were classified into 4 groups using the method described by Rodda et al. Visual observation-based classification (visual classification) was compared with classification by 3D analysis-based methods (3D classification). The reliabilities of visual classifications made by an experienced physician and a trainee physician were analyzed.
RESULTS
The consistency of inspection-based gait classification using kinematic data analysis was demonstrated by an experienced physician (Kappa coefficient (k)=0.67, p<0.001). However, the consistency was low for the trainee physician (k=0.37, p<0.001). Group III (apparent equinus) was commonly confused with group IV (crouch gait) by the trainee physician, resulting in lower agreement for those two evaluation groups than for other patterns. Video observation showed low reliability in comparisons made between the experienced and the trainee physician (k=0.37, p<0.001).
CONCLUSION
There was substantial agreement of gait classification between video observation and kinematic data analysis by the experienced physician, but not by the trainee physician. Low reliability was also demonstrated for inspection-based gait classification.
Keyword
Figure
Cited by 1 articles
-
Comment on “Effect of Extracorporeal Shockwave Therapy Versus Intra-articular Injections of Hyaluronic Acid for the Treatment of Knee Osteoarthritis”
Valter Santilli, Federica Alviti, Marco Paoloni, Massimiliano Mangone, Andrea Bernetti
Ann Rehabil Med. 2018;42(2):372-373. doi: 10.5535/arm.2018.42.2.372.
Reference
-
1. Rodda J, Graham HK. Classification of gait patterns in spastic hemiplegia and spastic diplegia: a basis for a management algorithm. Eur J Neurol. 2001; 8(Suppl 5):98–108. PMID: 11851738.
Article2. Winters TF Jr, Gage JR, Hicks R. Gait patterns in spastic hemiplegia in children and young adults. J Bone Joint Surg Am. 1987; 69:437–441. PMID: 3818706.3. O'Byrne JM, Jenkinson A, O'Brien TM. Quantitative analysis and classification of gait patterns in cerebral palsy using a three-dimensional motion analyzer. J Child Neurol. 1998; 13:101–108. PMID: 9535234.4. Kienast G, Bachmann D, Steinwender G, Zwick EB, Saraph V. Determination of gait patterns in children with cerebral palsy using cluster analysis. Gait Posture. 1999; 10:57.
Article5. Rodda JM, Graham HK, Carson L, Galea MP, Wolfe R. Sagittal gait patterns in spastic diplegia. J Bone Joint Surg Br. 2004; 86:251–258. PMID: 15046442.
Article6. DeLuca PA. Gait analysis in the treatment of the ambulatory child with cerebral palsy. Clin Orthop Relat Res. 1991; 264:65–75. PMID: 1997253.
Article7. Gage JR, DeLuca PA, Renshaw TS. Gait analysis: principle and applications with emphasis on its use in cerebral palsy. Instr Course Lect. 1996; 45:491–507. PMID: 8727765.8. Park ES, Rha DW, Kim HB, Kim MH. Common gait abnormalities of each joint in children with spastic cerebral palsy. J Korean Acad Rehabil Med. 2009; 33:64–71.9. Toro B, Nester CJ, Farren PC. Cluster analysis for the extraction of sagittal gait patterns in children with cerebral palsy. Gait Posture. 2007; 25:157–165. PMID: 16647260.
Article10. Mulroy S, Gronley J, Weiss W, Newsam C, Perry J. Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture. 2003; 18:114–125. PMID: 12855307.
Article11. Wren TA, Rethlefsen S, Kay RM. Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Orthop. 2005; 25:79–83. PMID: 15614065.12. Bartko JJ. Measures of agreement: a single procedure. Stat Med. 1994; 13:737–745. PMID: 8023046.
Article13. Rang M, Silver R, De La Garza J. Lovell WW, Winter RB, editors. Cerebral palsy. Pediatric orthopaedics. 1986. 2nd ed. Philadelphia: JB Lippincott Company;p. 345–396.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visual-perceptual Function in Children with Spastic Cerebral Palsy
- Kinematic Gait Analysis in Children with Hemiplegic Spastic Cerebral Palsy
- Kinematic Gait Analysis in Children with Spastic Diplegic Cerebral Palsy after Selective Posterior Rhizotomy: Long Term Follow Up
- Gait Patterns According to the Transverse Plane Deformities in Spastic Diplegia: A Preliminary Report
- Motor Point Block By Phenol in Spastic Cerebral Palsy