Ann Rehabil Med.
2011 Dec;35(6):791-797. 10.5535/arm.2011.35.6.791.
Improvement of Quiet Standing Balance in Patients with Wallenberg Syndrome after Rehabilitation
- Affiliations
-
- 1Department of Rehabilitation Medicine, Ewha Womans University School of Medicine, Seoul 158-710, Korea. yoonreha@ewha.ac.kr
- KMID: 2266804
- DOI: http://doi.org/10.5535/arm.2011.35.6.791
Abstract
OBJECTIVE
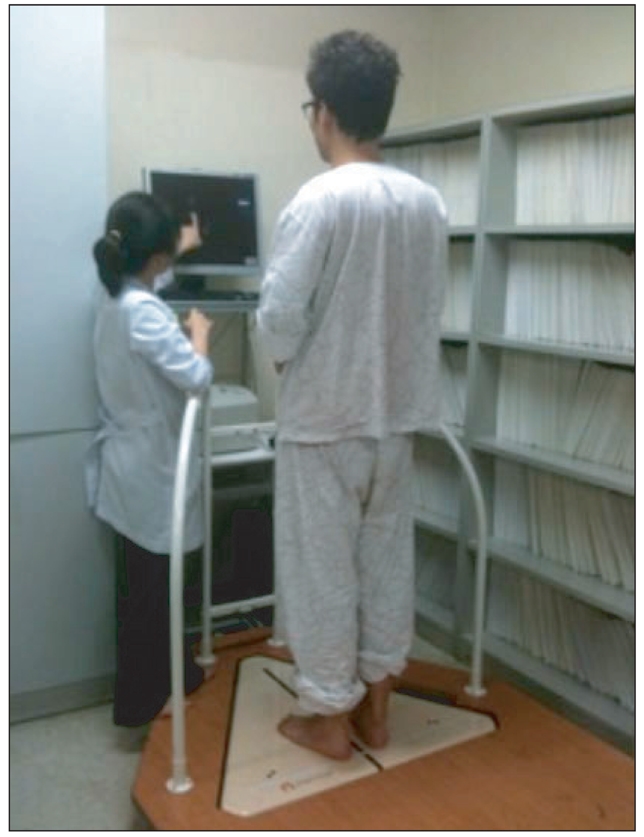
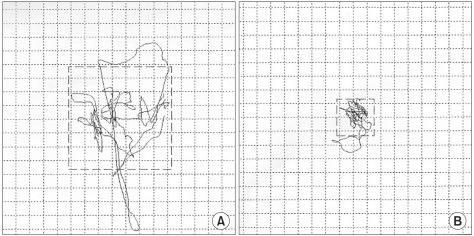
To evaluate quiet standing balance of patients with Wallenberg syndrome before and after rehabilitation. METHOD: Six patients with Wallenberg syndrome were enrolled within one month after being affected by an infarct of the lateral medulla. Quiet standing balance was assessed using posturography with eyes open and closed. The assessment was repeated after the patients had undergone rehabilitation treatment for three to nine months, and the results of the two assessments were compared.
RESULTS
The quiet standing balance evaluation was performed by measurement of center of pressure (CoP) movement. In the initial test, the mean scores of mediolateral and anteroposterior speed, velocity movement, mediolateral and anteroposterior extent of CoP were all high, indicating impairments of quiet standing balance in the patients. After rehabilitation treatment, the anteroposterior speed and extent, the mediolateral speed and extent, and velocity moment of CoP showed statistically significant reductions in the eyes open condition (p<0.05), and the anteroposterior speed and extent and velocity moment of CoP had decreased in the eyes closed condition (p<0.05). Mediolateral speed and extent of CoP in the eyes closed condition had also decreased, but the reduction was not statistically significant.
CONCLUSION
This study demonstrated improvements of quiet standing balance, especially anteroposterior balance, in patients with Wallenberg syndrome following rehabilitation. We suggest that balance training is important in the rehabilitation of Wallenberg syndrome and that, as an objective measure of balance status, posturography is useful in the assessment of quiet standing balance.
Keyword
MeSH Terms
Figure
Reference
-
1. Delisa JA, Gans BM, Walsh NE. Physical medicine & rehabilitation principles and practice. 2005. 4th ed. Philadelphia: Lippincott Williams and Wilkins;p. 1660.2. Lee SS, Roh JK, Lee SB, Myung HJ. A clinical study of 21 patients with lateral medullary syndrome. J Korean Neurol Assoc. 1989; 7:42–51.3. Lee KG, Chun MH, Kim BR, Kang SH. The effects of biofeedback balance training using interactive balance system in acute stroke patients. J Korean Acad Rehabil Med. 2009; 33:41–47.4. Kim HD, Kweon DC, Park IS, Im JJ, Nam SH, Park SJ. Quantitative measurement of postural sway during upright posture. J Korean Acad Rehabil Med. 1995; 19:495–499.5. Kim CR, Chun MH, Lee GA. Assessments of balance control using Tetra-ataxiametric posturography. J Korean Acad Rehabil Med. 2009; 33:429–435.6. Lim KB, Na YM, Lee HJ, Joo SJ. Comparison of postural control measures between older and younger adults using balance master system. J Korean Acad Rehabil Med. 2003; 27:418–423.7. Rha DW, Park CI, Chung HI, Kim MJ, Kim HB, Park ES. Comparison of postural control mechanisms during quiet standing between healthy children and children with spastic diplegic cerebral palsy. J Korean Acad Rehabil Med. 2006; 30:468–474.8. Lim KB, Lee HJ, Joo SJ, Lim SS. Postural control measures of patients with lower back pain using balance master system. J Korean Acad Rehabil Med. 2007; 31:30–36.9. Kim BR, Choi KH, Chun MH, Lee MC, Chung SJ, Jang KW. Evaluation of balance control in patients with idiopathic Parkinson's disease using Tetraataxiametric posturography. J Korean Acad Rehabil Med. 2009; 33:538–546.10. Kim HS, Lee KW, Sung DH, Hwang JH, Kim TU. Posturographic characteristics of lesion site in stroke patients. J Korean Acad Rehabil Med. 2000; 24:363–369.11. Kim SH, Seok H, Lee H, Lee HJ, Suh JW. The effects of transcutaneous electrical nerve stimulation for standing balance in patients with hemiplegia. J Korean Acad Rehabil Med. 2009; 33:159–164.12. Thapa PB, Gideon P, Brockman KG, Fought RL, Ray WA. Clincal and biomechanical measures of balance as fall predictors in ambulatory nursing home residents. J Gerontol A Biol Sci Med Sci. 1996; 51:M239–M246. PMID: 8808996.13. Lee H. Central nervous system disorders presenting as vertigo. J Korean Bal Soc. 2004; 3:95–101.14. Piirtola M, Era P. Force platform measurements as predictors of falls among older people-a review. Gerontology. 2006; 52:1–16. PMID: 16439819.15. Pajala S, Era P, Markku K, Jaakko K, Timo T, Taina R. Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling woman aged 63-76 years. J Gerontol A Biol Sci Med Sci. 2008; 63:171–178. PMID: 18314453.16. Berg K, Williams JI. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995; 27:27–36. PMID: 7792547.17. Yelnik A, Bonan I. Clinical tools for assessing balance disorder. Neurophysiol Clin. 2008; 38:439–445. PMID: 19026963.18. Gage WH, Winter DA. Kinematic and kinetic validity of the inverted pendulum model in quiet standing. Gait Posture. 2004; 19:124–132. PMID: 15013500.
Article19. Lehmann JF, Boswell S, Price R, Burleigh A, deLateur BJ, Jaffe KM, Hertling D. Quantitative evaluation of sway as an indicator of functional balance in post-traumatic brain injury. Arch Phys Med Rehabil. 1990; 71:955–962. PMID: 2241541.20. Winter DA, Patla AE. Motor mechanisms of balance during quiet standing. J Electromyogr Kinesiol. 2003; 13:49–56. PMID: 12488086.
Article21. Badke MB, Shea TA, Miedaner JA, Grove CR. Outcomes after rehabilitation for adults with balance dysfunction. Arch Phys Med Rehabil. 2004; 85:227–233. PMID: 14966706.
Article22. Kirsteins AE, Black-Schaffer RM, Harvey RL. Stroke rehabilitation. 3. Rehabilitation management. Arch Phys Med Rehabil. 1999; 80:S17–S20. PMID: 10326899.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Test Results and Standardized Method in Quiet Standing Balance Evaluation
- Effect of Hinged Ankle-Foot Orthoses on Standing Balance Control in Children with Bilateral Spastic Cerebral Palsy
- Sick Sinus Syndrome Combined with Wallenberg Syndrome: a Case Report
- Comparison of Postural Control Mechanisms during Quiet Standing between Healthy Children and Children with Spastic Diplegic Cerebral Palsy
- Evaluation of Standing Balance in Hemiplegic Patients Using the Functional Reach Test