Comparison of Treatment Goals for Moderate-to-Severe Psoriasis between Korean Dermatologists and the European Consensus Report
- Affiliations
-
- 1Department of Dermatology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. swyoun@snu.ac.kr
- 2Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Dermatology, Korea University College of Medicine, Seoul, Korea.
- 4Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea.
- 5Department of Dermatology, University of Ulsan College of Medicine, Seoul, Korea.
- 6Department of Dermatology, Kyung Hee University College of Medicine, Seoul, Korea.
- 7Department of Dermatology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 8Department of Dermatology, National Medical Center, Seoul, Korea.
- KMID: 2264808
- DOI: http://doi.org/10.5021/ad.2015.27.2.184
Abstract
- BACKGROUND
The development of therapies for psoriasis has led to the need for a new strategy to the treatment of patients with moderate-to-severe psoriasis. New consensus guidelines for psoriasis treatment have been developed in some countries, some of which have introduced treatment goals to determine the timing of therapeutic regimens for psoriasis.
OBJECTIVE
To investigate the opinions held by Korean dermatologists who specialize in psoriasis about treatment goals, and to compare these with the European consensus.
METHODS
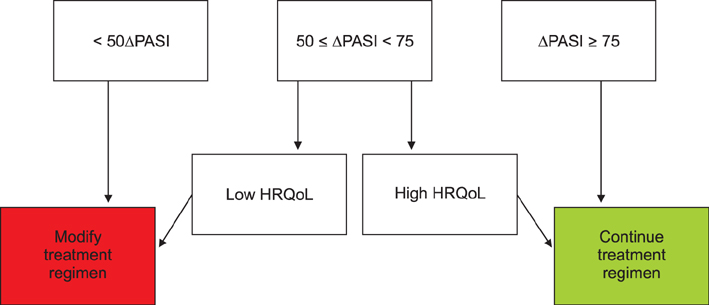
Korean dermatologists who specialize in psoriasis were asked 11 questions about defining the treatment goals for psoriasis. The questionnaire included questions about the factors used to classify the severity of psoriasis, defining the induction and maintenance phases of psoriasis treatment, defining treatment responses during the induction phase, and defining treatment responses during the maintenance phase.
RESULTS
The Korean consensus showed responses that were almost similar to the European consensus, even without using the Delphi technique, which uses repeated rounds of questions to reach a consensus. Only one response that related to psoriasis severity in the context of the quality of patients' lives differed from the European consensus.
CONCLUSION
The concept of using treatment goals in the treatment of moderate-to-severe psoriasis can be applied to Korean psoriasis patients. Since a tool for assessing the quality of patients' lives is not commonly used in Korea, the development of a simple, rapidly completed, and region-specific health-related quality of life assessment tool would enable treatment goals to be used in routine clinical practice.
MeSH Terms
Figure
Cited by 5 articles
-
The use of biologics for severe psoriasis
Sang Woong Youn
J Korean Med Assoc. 2015;58(10):917-922. doi: 10.5124/jkma.2015.58.10.917.The MARCOPOLO Study of Ustekinumab Utilization and Efficacy in a Real-World Setting: Treatment of Patients with Plaque Psoriasis in Asia-Pacific Countries
Sang Woong Youn, Tsen-Fang Tsai, Colin Theng, Siew-Eng Choon, Benny E. Wiryadi, Antonio Pires, Weihao Tan, Min-Geol Lee,
Ann Dermatol. 2016;28(2):222-231. doi: 10.5021/ad.2016.28.2.222.Severe Nail Fold Psoriasis Extending from Nail Psoriasis Resolved with Ustekinumab: Suggestion of a Cytokine Overflow Theory in the Nail Unit
Sang Young Byun, Bo Ri Kim, Jae Woo Choi, Sang Woong Youn
Ann Dermatol. 2016;28(1):94-97. doi: 10.5021/ad.2016.28.1.94.Could Psoriatic Arthritis Be Easily Diagnosed from Current Suspicious Physical Findings in the Dermatology Clinic?
Jee Woong Choi, Bo Ri Kim, Eunmi Seo, Sang Woong Youn
Ann Dermatol. 2017;29(1):48-54. doi: 10.5021/ad.2017.29.1.48.The Advantage of Cyclosporine A and Methotrexate Rotational Therapy in Long-Term Systemic Treatment for Chronic Plaque Psoriasis in a Real World Practice
Chong Won Choi, Bo Ri Kim, Jungyoon Ohn, Sang Woong Youn
Ann Dermatol. 2017;29(1):55-60. doi: 10.5021/ad.2017.29.1.55.
Reference
-
1. Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009; 361:496–509.
Article2. Galadari I, Sharif MO, Galadari H. Psoriasis: a fresh look. Clin Dermatol. 2005; 23:491–502.
Article3. Parisi R, Symmons DP, Griffiths CE, Ashcroft DM;; Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013; 133:377–385.
Article4. Hsu S, Papp KA, Lebwohl MG, Bagel J, Blauvelt A, Duffin KC, National Psoriasis Foundation Medical Board, et al. Consensus guidelines for the management of plaque psoriasis. Arch Dermatol. 2012; 148:95–102.
Article5. Pathirana D, Nast A, Ormerod AD, Reytan N, Saiag P, Smith CH, et al. On the development of the European S3 guidelines on the systemic treatment of psoriasis vulgaris: structure and challenges. J Eur Acad Dermatol Venereol. 2010; 24:1458–1467.
Article6. Ohtsuki M, Terui T, Ozawa A, Morita A, Sano S, Takahashi H, et al. Japanese guidance for use of biologics for psoriasis (the 2013 version). J Dermatol. 2013; 40:683–695.
Article7. Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, Chair of Guideline Group, et al. British Association of Dermatologists' guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009; 161:987–1019.
Article8. Kragballe K, Gniadecki R, Mørk NJ, Rantanen T, Ståhle M. Implementing best practice in psoriasis: a Nordic expert group consensus. Acta Derm Venereol. 2014; 94:547–552.
Article9. Mrowietz U, Kragballe K, Reich K, Spuls P, Griffiths CE, Nast A, et al. Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch Dermatol Res. 2011; 303:1–10.
Article10. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994; 19:210–216.
Article11. Finlay AY, Basra MK, Piguet V, Salek MS. Dermatology life quality index (DLQI): a paradigm shift to patient-centered outcomes. J Invest Dermatol. 2012; 132:2464–2465.
Article12. Gupta AK, Pandey SS, Pandey BL. Effectiveness of conventional drug therapy of plaque psoriasis in the context of consensus guidelines: a prospective observational study in 150 patients. Ann Dermatol. 2013; 25:156–162.
Article13. Lee YW, Park EJ, Kwon IH, Kim KH, Kim KJ. Impact of psoriasis on quality of life: relationship between clinical response to therapy and change in health-related quality of life. Ann Dermatol. 2010; 22:389–396.
Article14. Zweegers J, van den Reek JM, van de Kerkhof PC, Otero ME, Ossenkoppele PM, Njoo MD, et al. Comparing treatment goals for psoriasis with treatment decisions in daily practice: results from a prospective cohort of patients with psoriasis treated with biologics: BioCAPTURE. Br J Dermatol. 2014; 171:1091–1098.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Basic Therapeutic Approach for Patients with Plaque Psoriasis: Korean Expert Consensus Using the Modified Delphi Method
- A Study of Awareness and Screening Behavior of Cardiovascular Risk Factors in Patients with Psoriasis and Dermatologists
- Clinical Study on Psoriasis
- Clinical Study on Psoriasis - 2 . Classification of Severity and Comparative Study by the Activity of Psoriasis
- Adherence to Topical Therapies for the Treatment of Psoriasis: Surveys of Physicians and Patients