Korean J Hematol.
2007 Dec;42(4):409-413. 10.5045/kjh.2007.42.4.409.
A Case of Massive Intravascular Hemolysis Associated with Clostiridium perfringens Sepsis
- Affiliations
-
- 1Department of Laboratory Medicine, East-West Neo Medical Center, Kyung Hee University College of Medicine, Seoul, Korea. wileemd@khu.ac.kr
- KMID: 2252228
- DOI: http://doi.org/10.5045/kjh.2007.42.4.409
Abstract
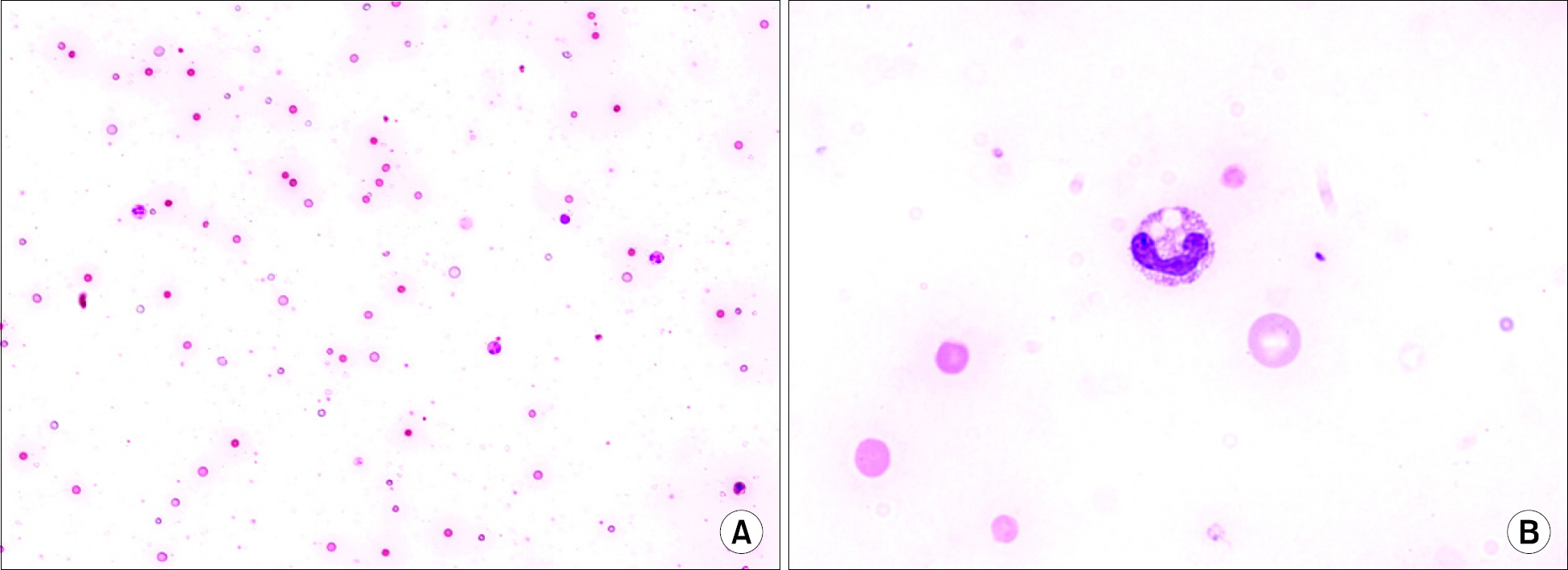
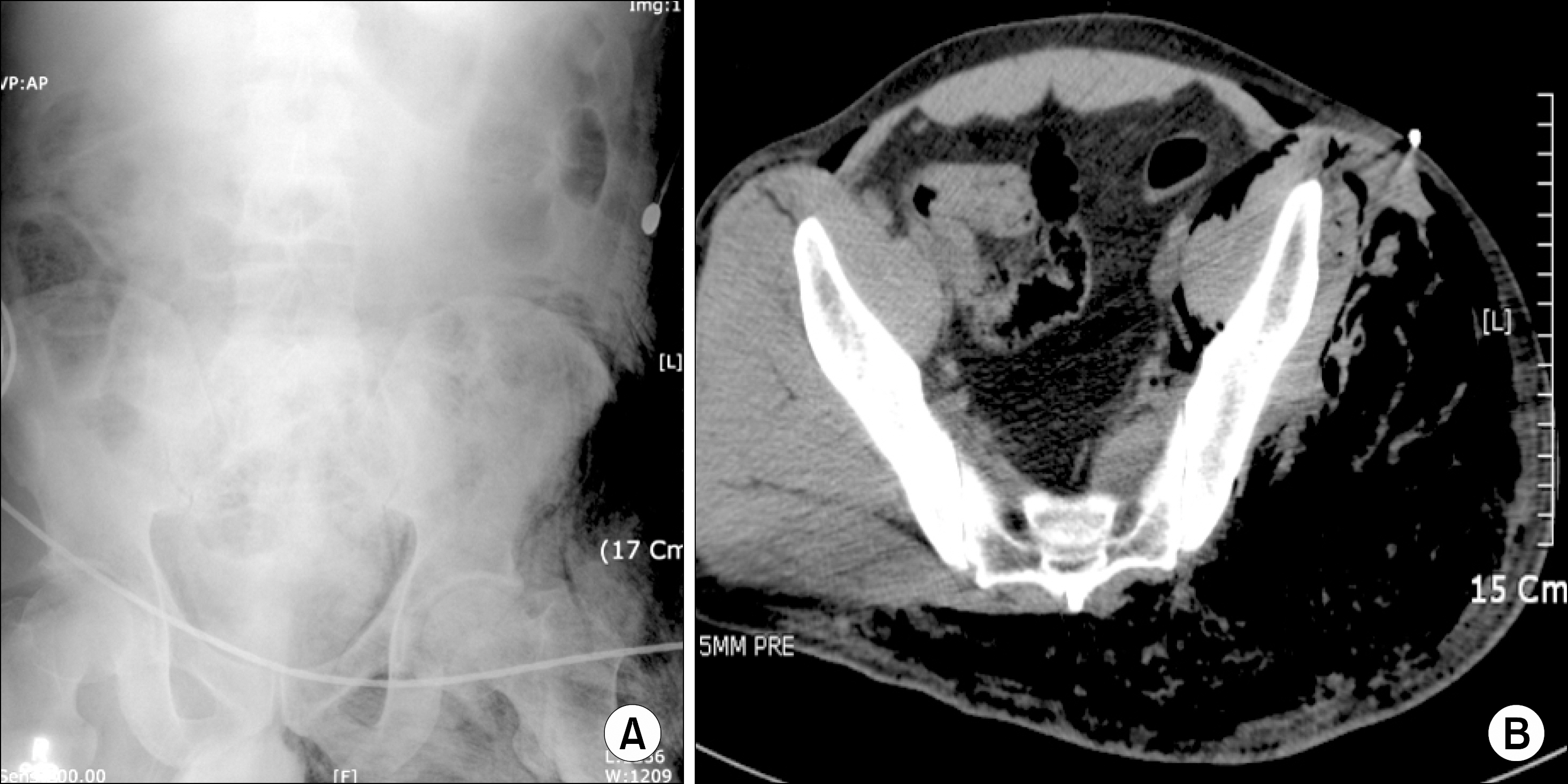
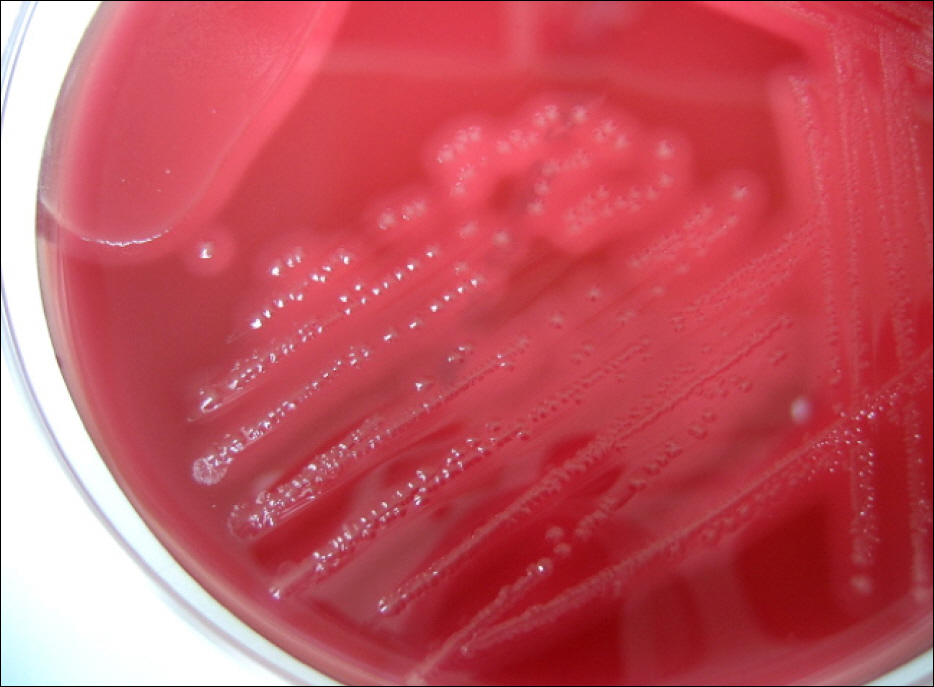
- Clostridium perfringens is an anaerobic, gram-positive rod that inhabits the soil and the intestinal tracts of many animals, including humans. C. perfringens is a major cause of food poisoning, traumatic or nontraumatic myonecrosis, clostridial cellulitis, gangrenous cholecystitis, sepsis or bacteremia, and intravascular hemolysis. Massive intravascular hemolysis is a rare complication of C. perfringens septicemia and has a high mortality rate with an extremely rapid progression. Therefore, aggressive treatment is required as soon as the diagnosis is made. In this study, we report a case of massive intravascular hemolysis due to C. perfringens septicemia in a 34-year-old man with liver cirrhosis.
MeSH Terms
Figure
Reference
-
1). Rechner PM., Agger WA., Mruz K., Cogbill TH. Clinical features of clostridial bacteremia: a review from a rural area. Clin Infect Dis. 2001. 33:349–53.
Article2). Haddy RI., Nadkarni DD., Mann BL, et al. Clostridial bacteremia in the community hospital. Scand J Infect Dis. 2000. 32:27–30.3). Vaiopoulos G., Calpadaki C., Sinifakoulis H, et al. Massive intravascular hemolysis: a fatal complication of Clostridium perfringens septicemia in a patient with acute myeloid leukemia. Leuk Lymphoma. 2004. 45:2157–9.
Article4). McArthur HL., Dalal BI., Kollmannsberger C. Intravascular hemolysis as a complication of Clostridium perfringens sepsis. J Clin Oncol. 2006. 24:2387–8.
Article5). Loran MJ., McErlean M., Wilner G. Massive hemolysis associated with Clostridium perfringens sepsis. Am J Emerg Med. 2006. 24:881–3.
Article6). Batge B., Filejski W., Kurowski V., Kluter H., Djonlagic H. Clostridial sepsis with massive intravascular hemolysis: rapid diagnosis and successful treatment. Intensive Care Med. 1992. 18:488–90.
Article7). Kuroda S., Okada Y., Mita M, et al. Fulminant massive gas gangrene caused by Clostridium perfringens. Intern Med. 2005. 44:499–502.
Article8). Abella BS., Kuchinic P., Hiraoka T., Howes DS. Atraumatic clostridial myonecrosis: case report and literature review. J Emerg Med. 2003. 24:401–5.
Article9). Poulou A., Manolis EN., Markou F., Ropotos A., Georgiadis M., Tsakris A. Fatal massive hemolysis as the first manifestation of Clostiridium perfringens septicemia in patient with non-systemic or local predisposing disorder. Anaerobe. 2007. 13:40–2.10). Singer AJ., Migdal PM., Oken JP., Chale SN., Moll UM. Clostridium perfringens septicemia with massive hemolysis in a patient with Hodgkin's lymphoma. Am J Emerg Med. 1997. 15:152–4.
Article11). Titball RW., Naylor CE., Basak AK. The Clostridium perfringens alpha-toxin. Anaerobe. 1999. 5:51–64.12). Stevens DL., Bryant AE. The role of clostridial toxins in the pathogenesis of gas gangrene. Clin Infect Dis. 2002. 35(1 Suppl):93–100.
Article13). Chen YM., Lee HC., Chang CM., Chuang YC., Ko WC. Clostridium bacteremia: emphasis on the poor prognosis in cirrhotic patients. J Microbiol Immunol Infect. 2001. 34:113–8.14). Ohtani S., Watanabe N., Kawata M., Harada K., Himei M., Murakami K. Massive intravascular hemolysis in a patient infected by a Clostridium perfringens. Acta Med Okayama. 2006. 60:357–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Clostridium perfringens Septicemia with Fatal Hemolytic Complication
- A Fulminant Case of Clostridium perfringens Septic Shock caused by a Liver Abscess with Massive Hemolytic Anemia
- Morganella Morganii Sepsis with Massive Hemolysis
- Massive intravascular hemolysis associated with Clostridium perfringens bacteremia
- Death due to Sepsis in Emphysematous Cholecystitis